A 75-year-old male presents with progressive generalized muscle weakness, issues with balance, back pain, as well as numbness and tingling in the bottom of his feet. Physical exam shows motor strength 4+/5 with good tone and without atrophy, asymmetry, or fasciculations. Hand grip and hip flexor strength is decreased. Shoulder girdle strength is stable. Sensory exam shows decreased proprioception, vibration, and light touch. The patient’s past medical history includes peripheral neuropathy, type 2 diabetes mellitus, hyperlipidemia, and hypertension. Prior alcohol use is reported. EMG/NCS shows electrodiagnostic findings of polyneuropathy. CPK is reportedly in the normal range. Skeletal muscle biopsy is pursued. What is the diagnosis of the myopathy pictured below in figure 1?
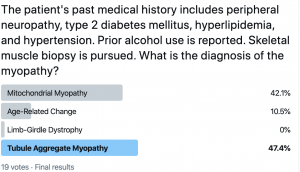
Frozen sections of skeletal muscle with Tubular Aggregate Myopathy (TAM) demonstrating two adjacent muscle fibers with round to ovoid eccentric basophilic (blue) inclusions (Figure 1) with routine hematoxylin and eosin (H&E) stain, other scattered muscle fibers show occasional inclusions in central to subsarcolemmal locations (not shown in Figure 1), and co-localization of the same two adjacent muscle fibers on deeper section show inclusion material with dense bright fuchsinophilic (red) staining character (Figure 2) with modified Gomori Trichrome (MGT) preparation. (H&E and MGT stains: original magnification 400x, each).
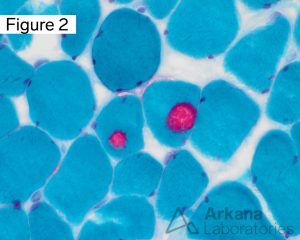
Answer: The muscle biopsy demonstrates occasional scattered muscle fibers with tubular aggregates, myopathy with tubular aggregates (i.e. tubular aggregate myopathy, TAM). Tubular aggregates are not specific as to etiology as they may be seen in a variety of both acquired and inherited conditions. The descriptive diagnosis we typically render is “Myopathy with Tubular Aggregates” which correlates to Tubular Aggregate Myopathy. The exact spelling of the answer choice was altered to accommodate the Twitter platform’s poll character limit. The acquired conditions include alcoholic myopathy, periodic paralysis (hypo-, hyper-, normokalemic, and thyrotoxic), neuropathy, motor neuron disease, inflammatory myopathy, and acromegaly. Tubular aggregates have also been seen in the setting of phosphoglycerate mutase deficiency (PGAM1 gene), limb-girdle myasthenia associated with GFPT1 mutations, and myotonic dystrophy.
Cases with frequent aggregates on biopsy are classified as “tubular aggregate myopathy (TAM)”. Recently, mutations in two genes, STIM1 and ORAI1, have been identified in familial cases of TAM, but these cases typically present in younger patients.
Four phenotypes have been described: (1) TAM with isolated progressive muscle weakness, (2) TAM with exercise-induced cramps, pain, and stiffness; (3) TAM with myasthenic features, and (4) TAM with gyrate atrophy of the choroids and retina. Other less commonly reported clinical manifestations in TAM patients include malignant hyperthermia and acute respiratory failure.
Why were the other answers incorrect?
The muscle biopsy demonstrates myopathy with tubular aggregates, and while the inclusions are fuchsinophilic with modified Gomori Trichrome (MGT) preparation, they are not composed of mitochondria. The muscle fibers do not show the typical morphology of ragged red fibers, as may be seen in a primary mitochondrial myopathy (answer choice A).
Age-related findings (answer choice B) may include a few rare early ragged red fibers in an elderly patient. The morphologic findings of myopathy with tubular aggregates are not that of mitochondrial pathology.
Tubular aggregates have been described in limb-girdle myasthenia associated with GFPT1 mutations, not limb-girdle muscular dystrophy (answer choice C). The pathologic findings of myopathy with tubular aggregates do not typically include pronounced dystrophic characteristics.
References:
Böhm J, Chevessier F, Koch C, et al. Clinical, histological and genetic characterization of patients with tubular aggregate myopathy caused by mutations in STIM1. J Med Genet. 2014 Dec;51(12):824-33. PMID: 25326555.
De Paula AM, Bartoli M, Courrier S, et al. Further heterogeneity in myopathy with tubular aggregates? Muscle Nerve. 2012 Dec;46(6):984-5. PMID: 23225398.
Endo Y, Noguchi S, Hara Y, et al. Dominant mutations in ORAI1 cause tubular aggregate myopathy with hypocalcemia via constitutive activation of store-operated Ca2+ channels. Hum Mol Genet. 2015 Feb 1;24(3):637-48. PMID: 25227914.
Naini A, Toscano A, Musumeci O, et al. Muscle phosphoglycerate mutase deficiency revisited. Arch Neurol. 2009 Mar;66(3):394-8. PMID: 19273759.
Neuromuscular website WUSTL: “http://neuromuscular.wustl.edu/musdist/lg.html#tub”
Nesin V, Wiley G, Kousi M, et al. Activating mutations in STIM1 and ORAI1 cause overlapping syndromes of tubular myopathy and congenital miosis. Proc Natl Acad Sci U S A. 2014 Mar 18;111(11):4197-202. PMID: 24591628.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.


