About Us
Arkana is a learning, teaching, innovating practice with one unifying passion: to work toward research breakthroughs that make our services unnecessary.
Learn About Our PracticePopular Posts

Kidneys for Kids
What are the kidneys and what do they do? Your kidneys are organs shaped like beans (think kidney beans) and…
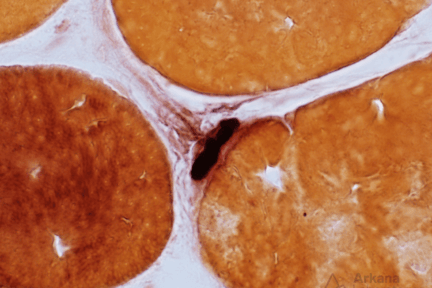
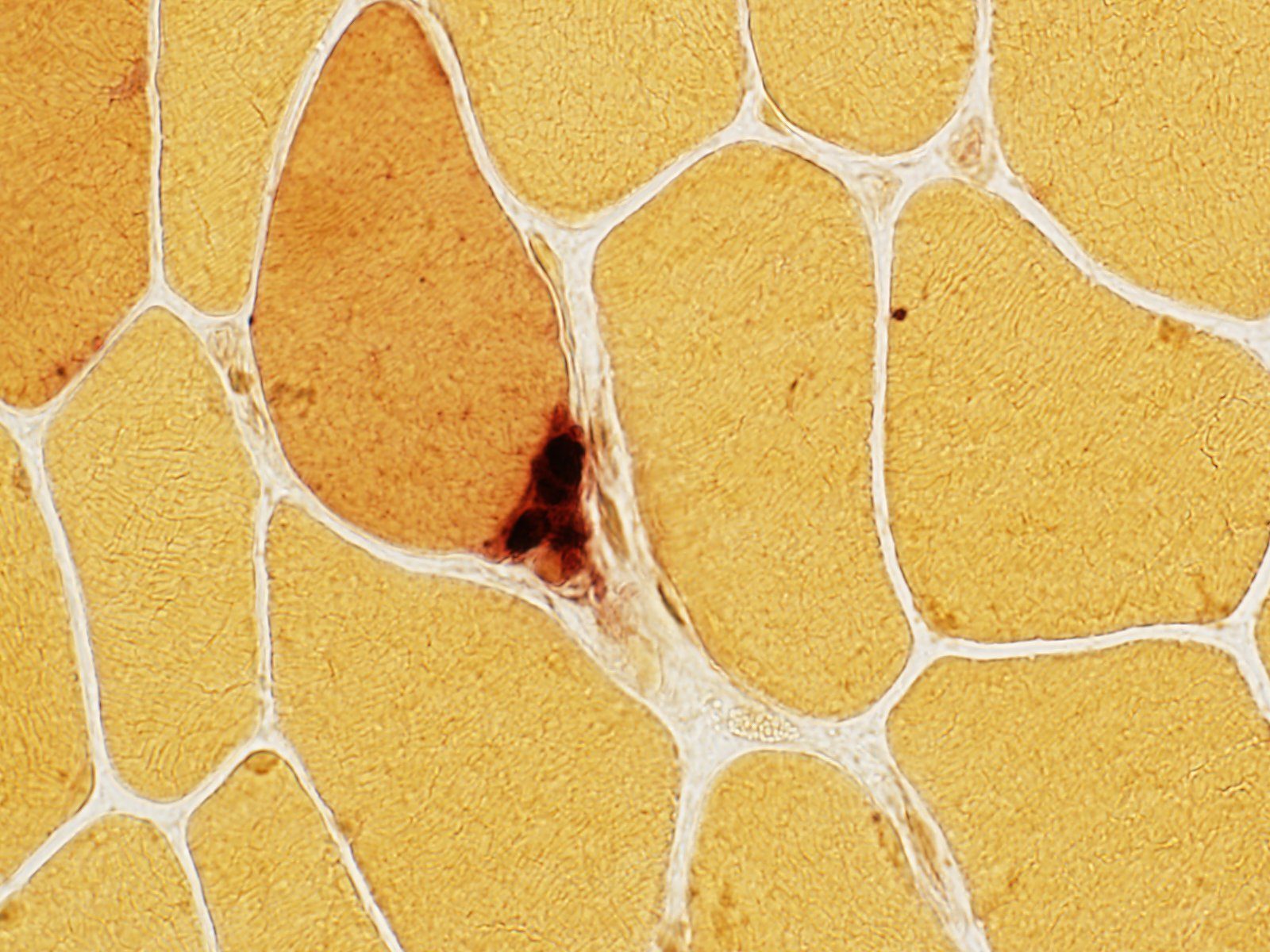
The Neuromuscular Junction
What is the dark staining structure? (Hint: note the small nerve twig associated with the structure). The neuromuscular junction (NMJ;…
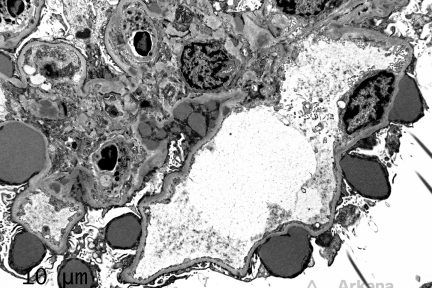
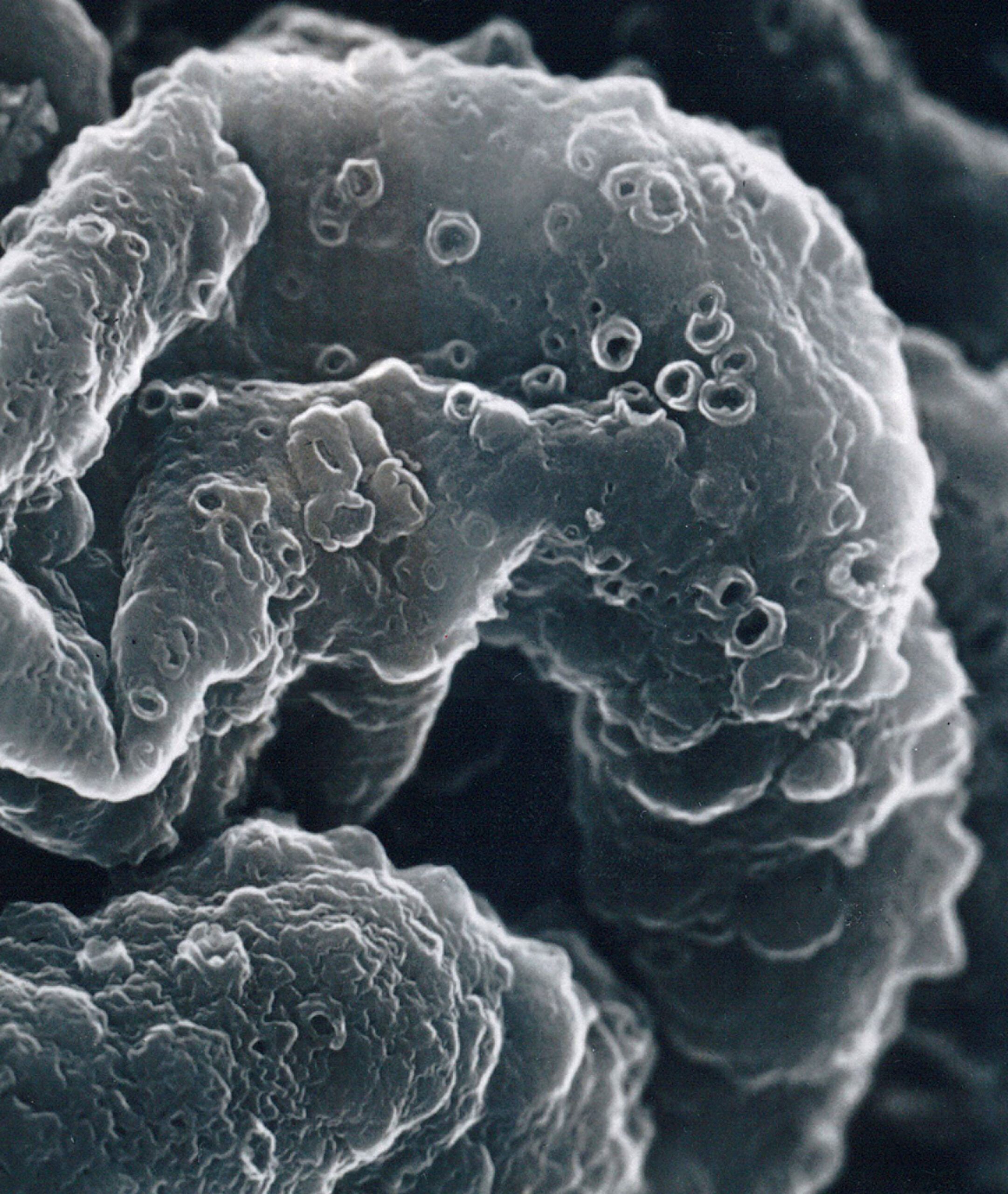
Subepithelial Humps
The depicted electron micrograph shows numerous, large and irregular subepithelial deposits which protrude from the glomerular basement membrane towards…
Diagnose This!
Diagnose This 4/29/2024
What would be your leading Dx and subtype based on the Congo red image above showing deposition predominately in the…
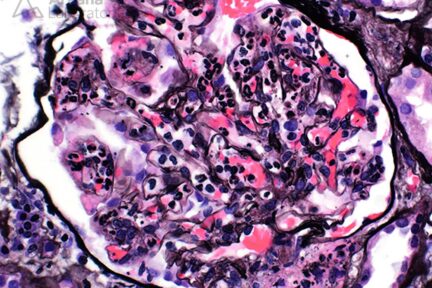
Diagnose This 4/15/2024
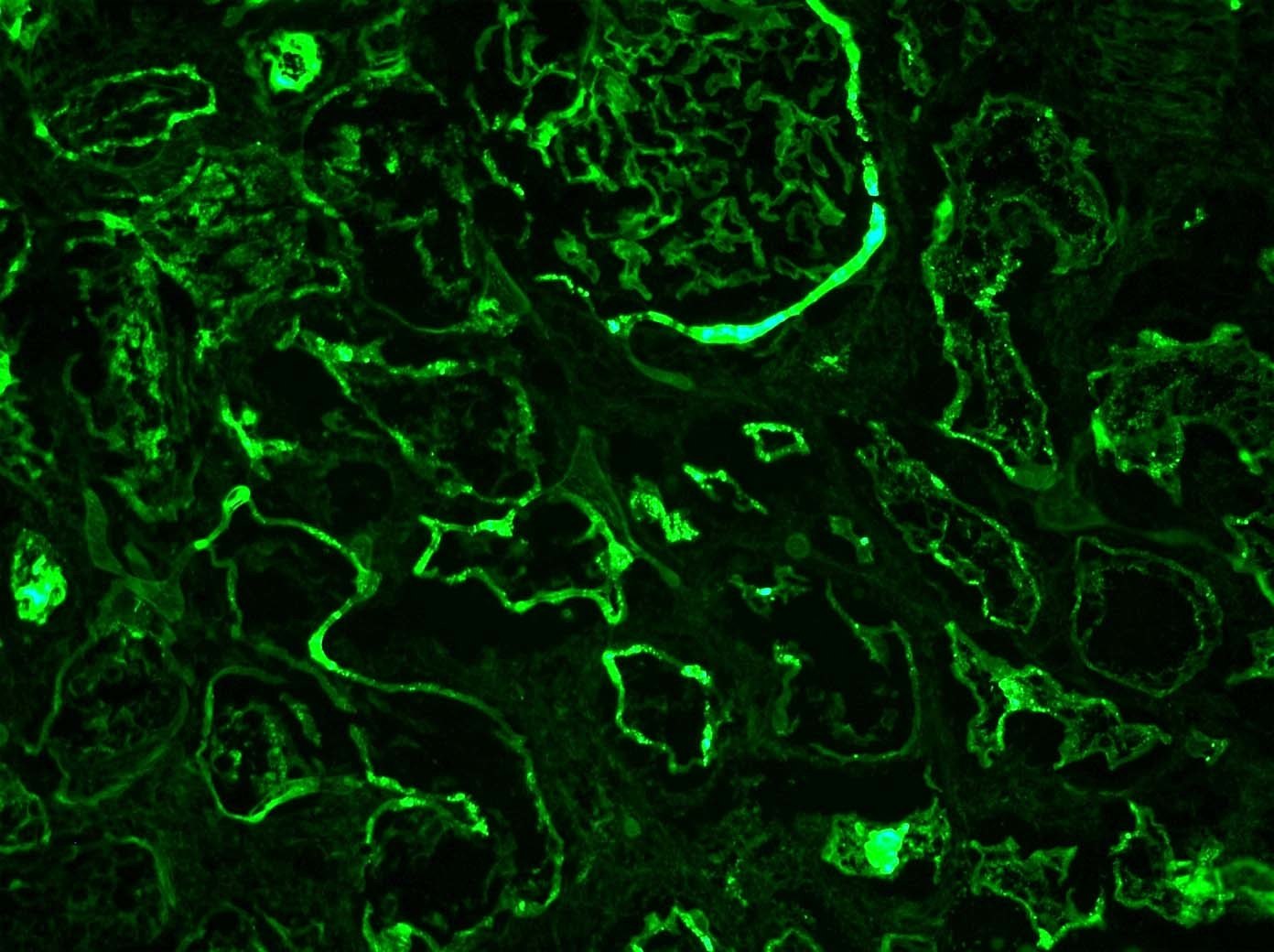
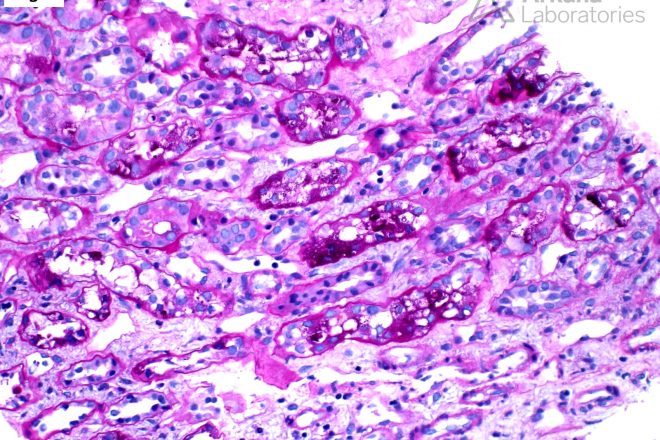
Based on the image provided, what would be your leading diagnosis with C3-dominant immune-complex deposition? The light microscopic image depicts…
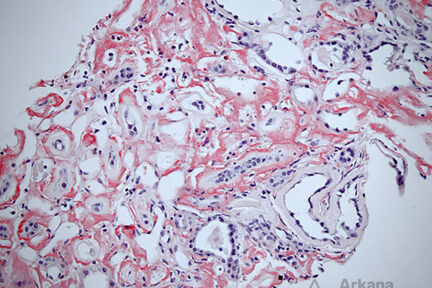
Diagnose This 4/1/2024
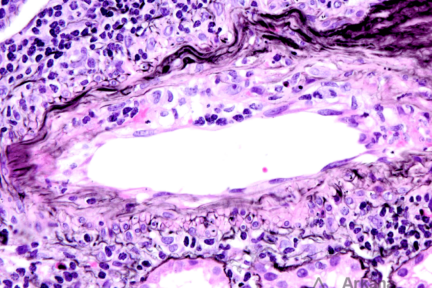
What is this finding and what is the significance in the transplant setting? The light microscopic image depicts an…
Podcast Episodes
Popular Subjects
Search & Filter All Posts