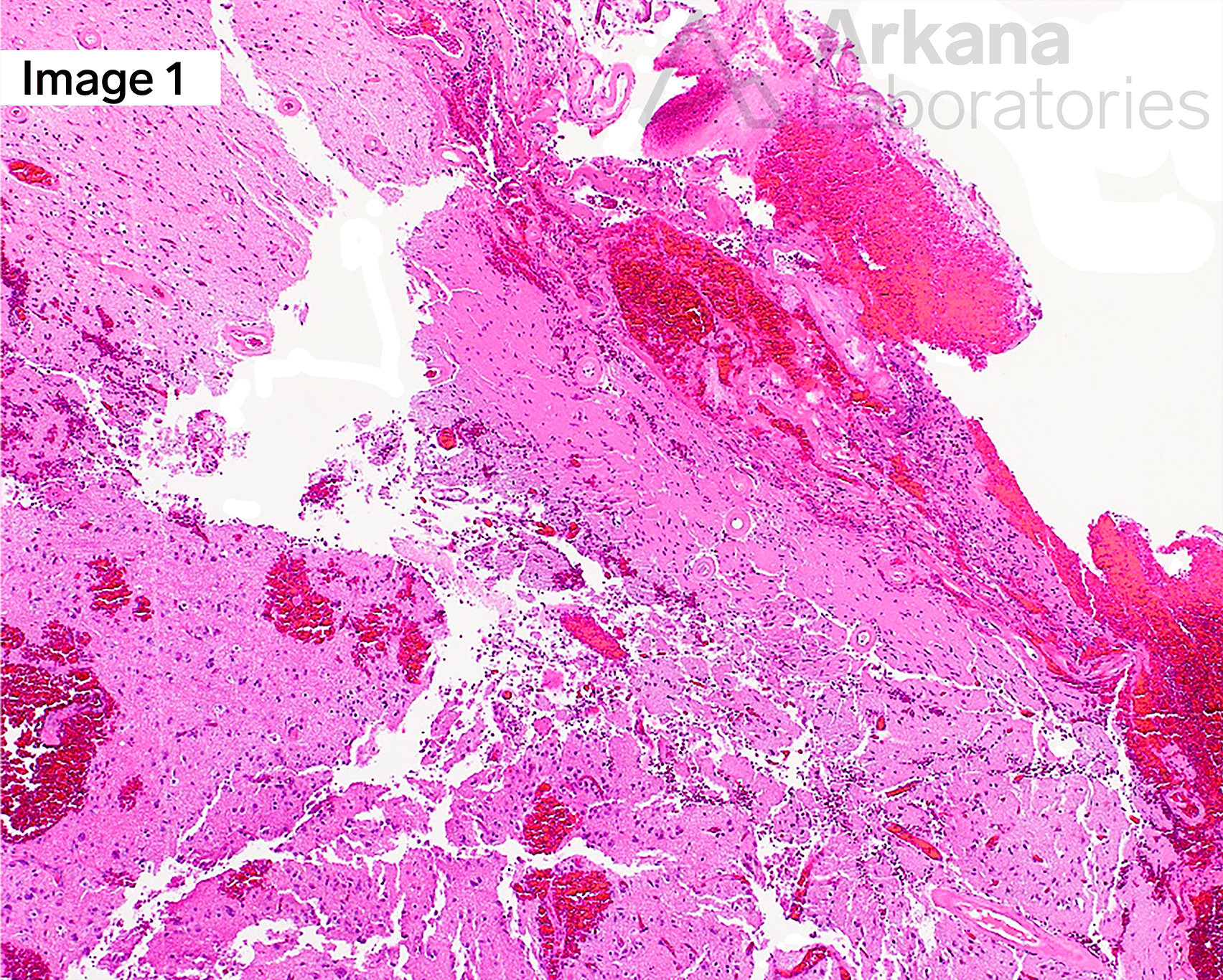
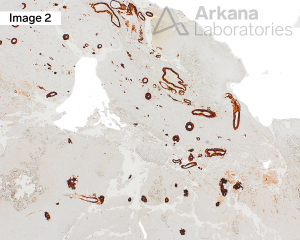
The patient is a male in his 7th decade who presents with left occipital hemorrhagic stroke. The patient has a history of a right frontotemporal stroke from which he made an excellent recovery. The patient lives in an assisted living facility and also has mild cognitive issues, which were not of certain to the patient or family. Resection specimen from the left occipital lesion (A) shows acute hemorrhage, reactive astrogliosis, and thickened intraparenchymal, as well as thickened leptomeningeal, blood vessel walls. A few scattered senile plaques (diffuse and neuritic) are also observed in the background. Aβ-amyloid deposition in the blood vessel walls is confirmed by immunostain (B). In addition, immunohistochemical (IHC) stain for Aβ-amyloid also highlights background plaques. (Original magnifications: A. FFPE H&E and B. IHC stain for Aβ-amyloid, 40x each)
Using the figures, which of the following is the diagnosis for this patient’s neuropathology?
Answer: Amyloid Angiopathy CAA
Cerebral amyloid angiopathy (CAA), choice (A), is a cerebrovascular disease of the elderly that results in spontaneous, synchronous or metachronous, cerebral lobar hemorrhage (CLH), as well as intracerebral hemorrhage (ICH), cerebral infarcts, and leukoencephalopathy.
Soluble Aβ-amyloid deposition in the vascular wall results in deterioration of vessel tunica media and narrowing of the vessel lumen. Cerebral arterioles lose ability to control blood flow in response to regional brain activation, resulting in decreased cerebral perfusion and impairment of the blood brain barrier (BBB). Amyloid is also know to cause vasoconstriction of cerebral vessels.
CAA can occur sporadically or in association with Alzheimer disease-type change neuropathology, as was seen in this case. CAA-type findings in a younger patient may be a clue to a familial disorder. No inflammation was seen in association with this case.
Why were the other answers wrong?
The pathologic findings of Diffuse Lewy body disease (DLBD) (Lewy body dementia), answer choice (B), are not seen in this case, and the clinical vignette is not typical for DLBD (i.e. parkinsonism, hallucinations, etc). DLBD is the second most common neurodegenerative disease after Alzheimer disease (AD).
Features of malignancy, either primary, GBM answer choice (C), or metastatic are not present.
The vessels in this case are abnormal, but are not malformative (i.e. back to back), as would be seen in a vascular malformation, answer choice (D).
References
Consensus recommendations for the postmortem diagnosis of Alzheimer’s disease. The National Institute on Aging, and Reagan Institute Working Group on Diagnostic Criteria for the Neuropathological Assessment of Alzheimer’s Disease. Neurobiol Aging. 1997 Jul-Aug;18(4 Suppl):S1-2. PMID: 9330978.
Corovic A, Kelly S, Markus HS. Cerebral amyloid angiopathy associated with inflammation: A systematic review of clinical and imaging features and outcome. Int J Stroke. 2018 Apr;13(3):257-267. PMID: 29134927.
DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener. 2019 Aug 2;14(1):32. PMID: 31375134.
Hyman BT, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 2012 Jan;8(1):1-13. PMID: 22265587.
Revesz T, Holton JL, Lashley T, et al. Genetics and molecular pathogenesis of sporadic and hereditary cerebral amyloid angiopathies. Acta Neuropathol. 2009 Jul;118(1):115-30. PMID: 19225789.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.