This 60-year-old patient presented with a several year history of slowly progressive proximal lower extremity weakness and mild elevation of CPK (300 range). Family history is negative for neuromuscular disorder. Serologic testing for cN-1A (NT5C1A) autoantibodies is positive. Myositis specific autoantibody testing is otherwise negative. More recently the patient has noticed some weakness of hand grip.
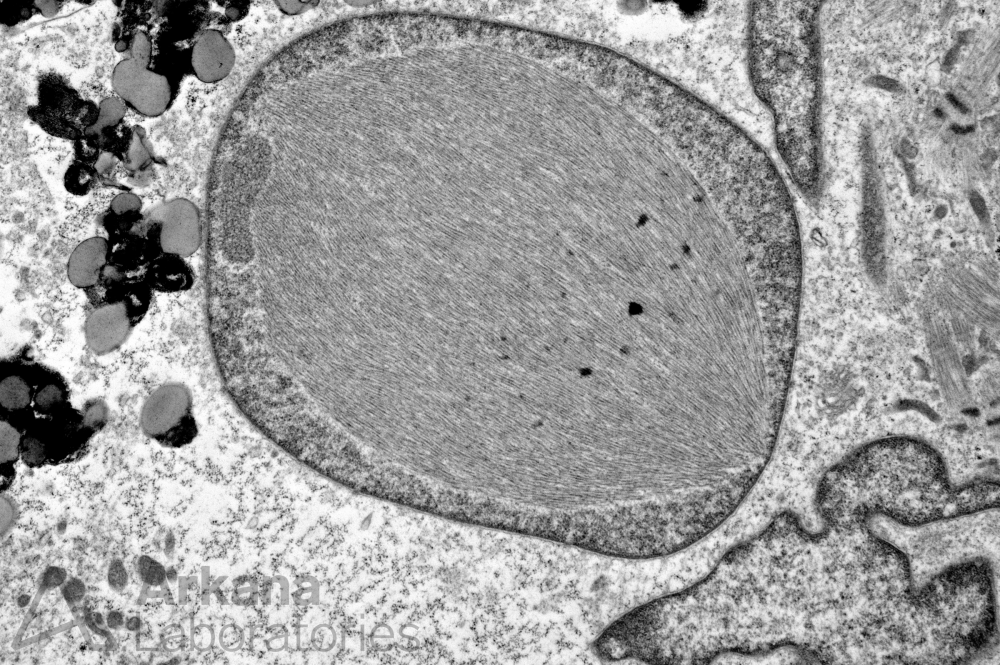
Based on the clinical history and electron microscopic finding in figure #1 which of the following diagnoses is most likely?
A. sIBM
B. Polymyositis
C. Anti-synthetase syndrome
D. Dermatomyositis
Correct answer: sIBM
The clinical features (patient age greater than 50 years, chronic progressive proximal lower extremity muscle weakness and distal upper extremity muscle weakness, mild elevation of CPK and positive cN-1A autoantibodies) along with the finding of intranuclear amyloid-like fibrillary inclusions on electron microscopy are consistent with the diagnosis of sporadic Inclusion Body Myositis (sIBM).
Features on light microscopy to keep an eye out for include polymyositis-like distribution of chronic inflammation, rimmed-vacuoles, congophilic intracellular inclusions, TDP43 and p62 positive protein aggregates. sIBM typically does not respond to treatment.
Rimmed-vacuoles and congophilic-TDP43-p62 positive inclusions are not specific to sIBM (i.e. may be seen in several other disease entities).
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.
