The patient is a 40-year-old who presented with proximal upper and lower extremity muscle weakness, and was found to have elevated CPK (600 range), negative myositis specific autoantibody panel test results, and myopathic features on EMG. They were treated with prednisone for clinically diagnosed polymyositis, and showed subsequent marked improvement in muscle strength and normalization of CPK levels.
One month later the patient was admitted to the hospital with recurrent weakness, shortness of breath, abdominal pain, nausea and vomiting of three days duration. A vastus lateralis muscle biopsy was performed.
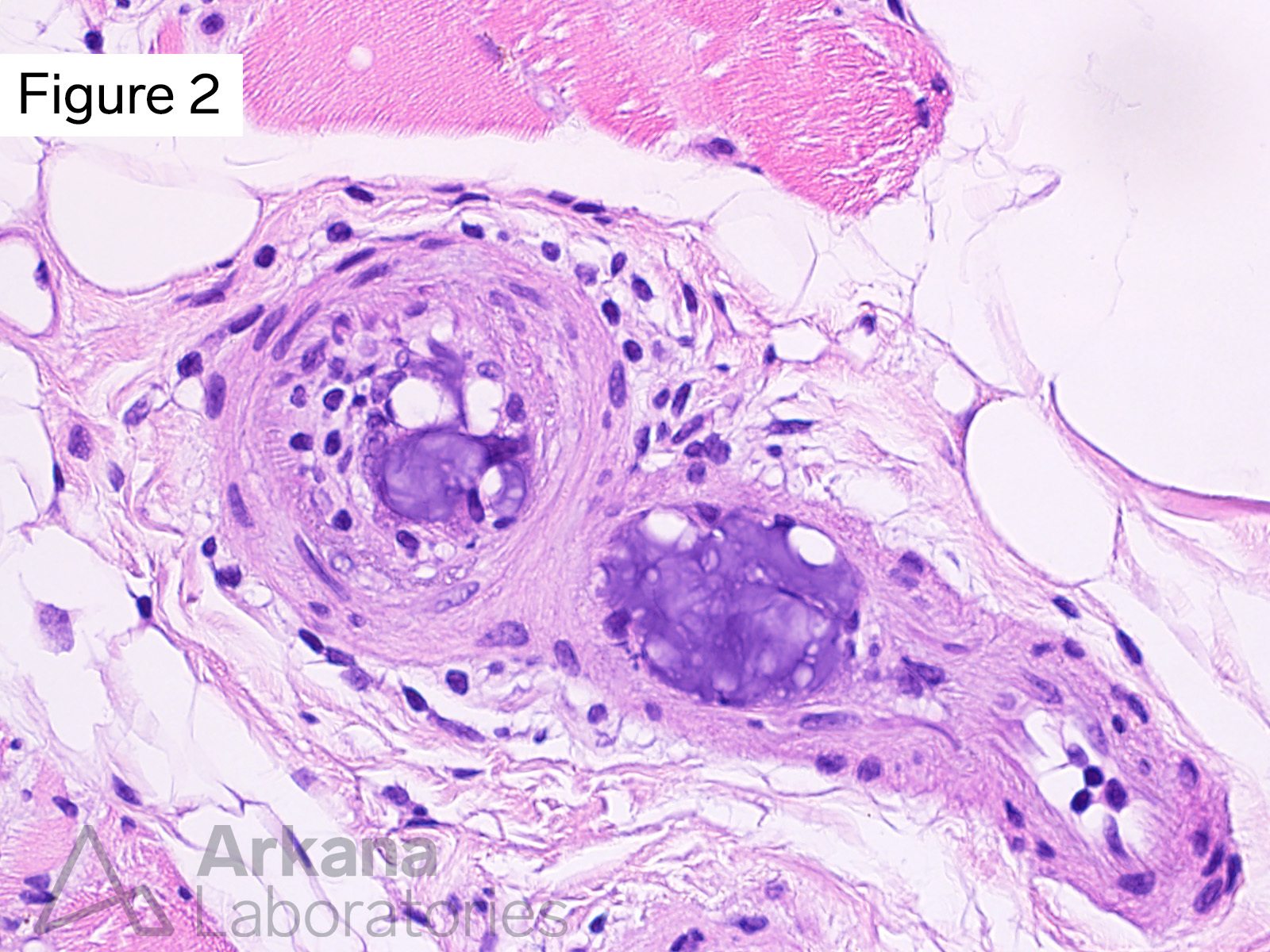
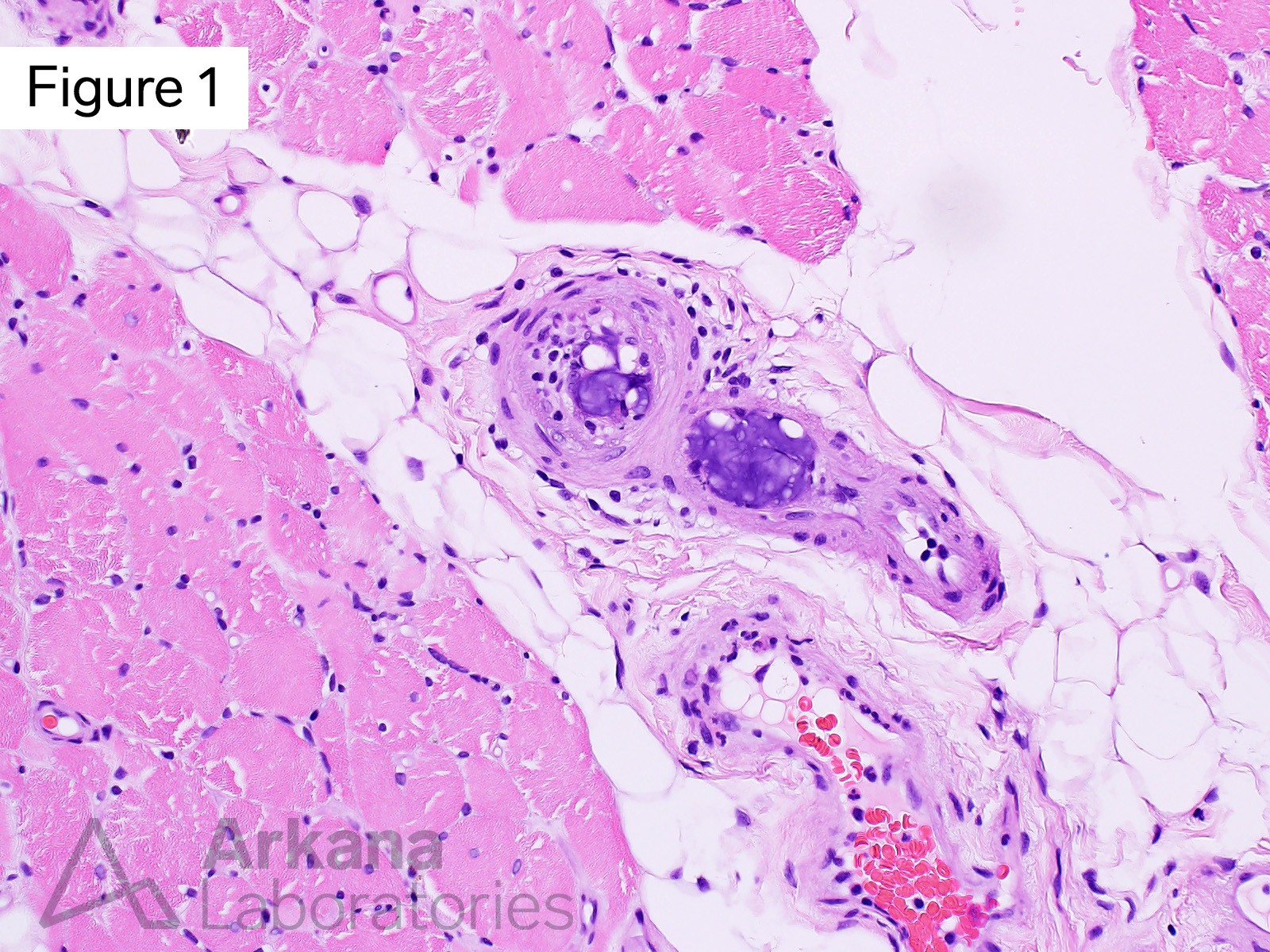
What of the following best describes the bluish material in Figures #1 and #2?
A. Foreign body emboli
B. Parasite
C. Granuloma
D. Stain artifact
Correct Answer: Foreign body emboli
The intravascular material is most consistent with foreign body embolic material. Hydrophilic polymer emboli (dislodged endovascular device coating) is felt to be most likely (please see references / additional reading). The possibility of embolic nucleus pulposis (intervertebral disc) was considered but is thought to be less likely.
Reference(s)/additional reading
Mehta RI, et al. Hydrophilic polymer embolism and associated vasculopathy of the lung: prevalence in a retrospective autopsy study. Hum Pathol. 2015 Feb;46(2):191-201. doi: 10.1016/j.humpath.2014.09.011. Epub 2014 Oct 7. PMID: 25543660; PMCID: PMC4552330.
Mehta RI, et al. Hydrophilic polymer emboli: an under-recognized iatrogenic cause of ischemia and infarct. Mod Pathol. 2010 Jul;23(7):921-30. doi: 10.1038/modpathol.2010.74. Epub 2010 Mar 19. PMID: 20305613.
Chopra AM, Mehta M, Bismuth J, Shapiro M, Fishbein MC, Bridges AG, Vinters HV. Polymer coating embolism from intravascular medical devices – a clinical literature review. Cardiovasc Pathol. 2017 Sep-Oct;30:45-54. doi: 10.1016/j.carpath.2017.06.004. Epub 2017 Jun 22. PMID: 28759819.
Kan I, et al. Microcatheter Originating Debris during Neuroendovascular Procedures: Mechanism of Dislodgement and Its Prevention. AJNR Am J Neuroradiol. 2020 Oct;41(10):1879-1881. doi: 10.3174/ajnr.A6723. Epub 2020 Aug 27. PMID: 32855184; PMCID: PMC7661062.
Sequeira A, Parimoo N, Wilson J, Traylor J, Bonsib S, Abreo K. Polymer embolization from minimally invasive interventions. Am J Kidney Dis. 2013 Jun;61(6):984-7. doi: 10.1053/j.ajkd.2012.12.021. Epub 2013 Feb 9. PMID: 23403021.
AbdelRazek MA, Mowla A, Farooq S, Silvestri N, Sawyer R, Wolfe G. Fibrocartilaginous embolism: a comprehensive review of an under-studied cause of spinal cord infarction and proposed diagnostic criteria. J Spinal Cord Med. 2016;39(2):146-54. doi: 10.1080/10790268.2015.1116726. Epub 2015 Dec 17. PMID: 26833287; PMCID: PMC5072491.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.