Clinical History:
This 40-year-old patient presented with complaints of muscle weakness and myalgias of approximately 3-months duration. Laboratory studies showed elevated CPK. Their past medical history is significant for interstitial lung disease. On physical examination, the patient was noted to have thickening and cracking of the skin of their fingers (Mechanic’s hands). Myositis specific autoantibody panel test results are pending.
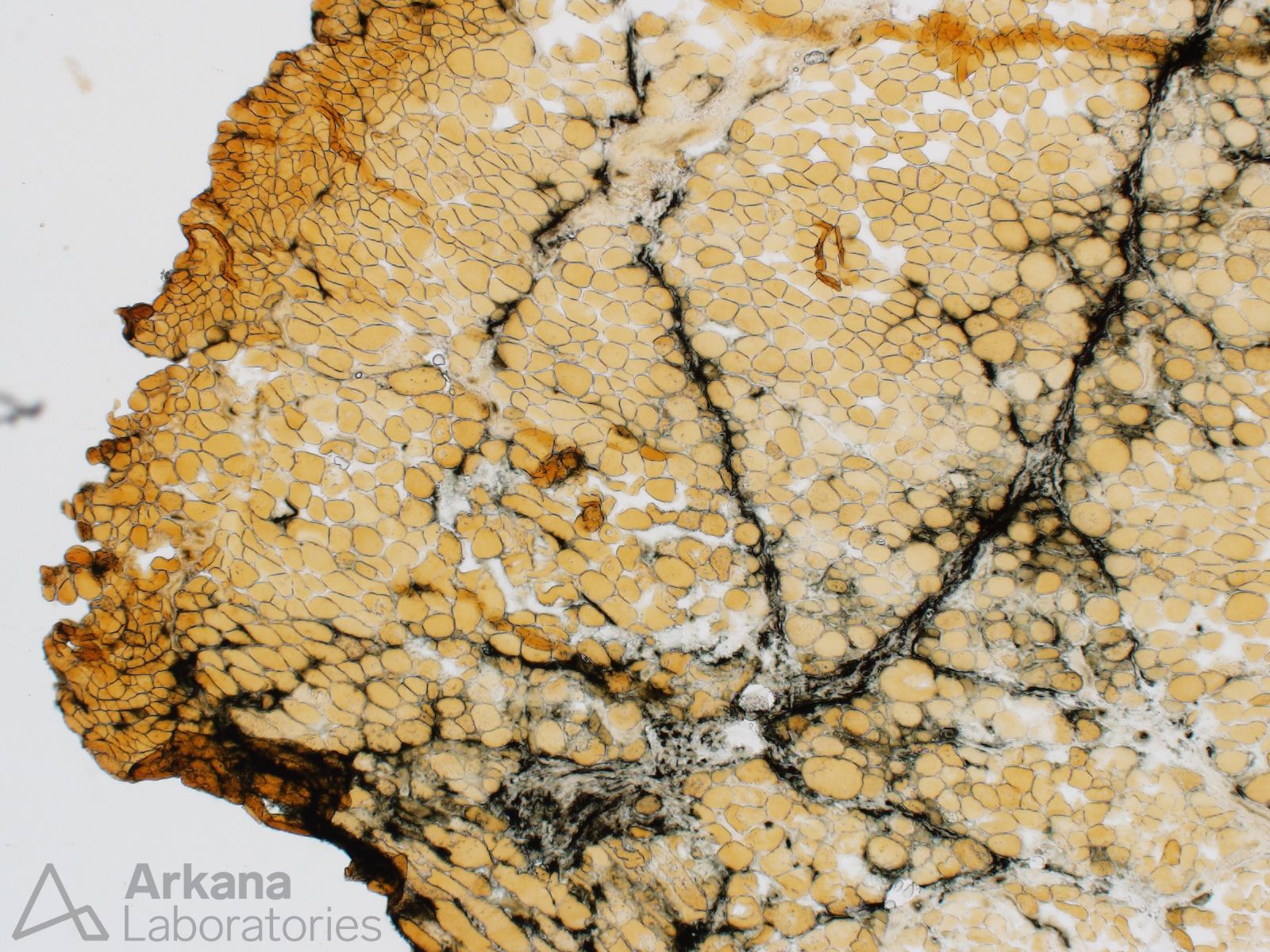
What information does the alkaline phosphatase enzyme histochemical stain (Image #1) provide on this case?
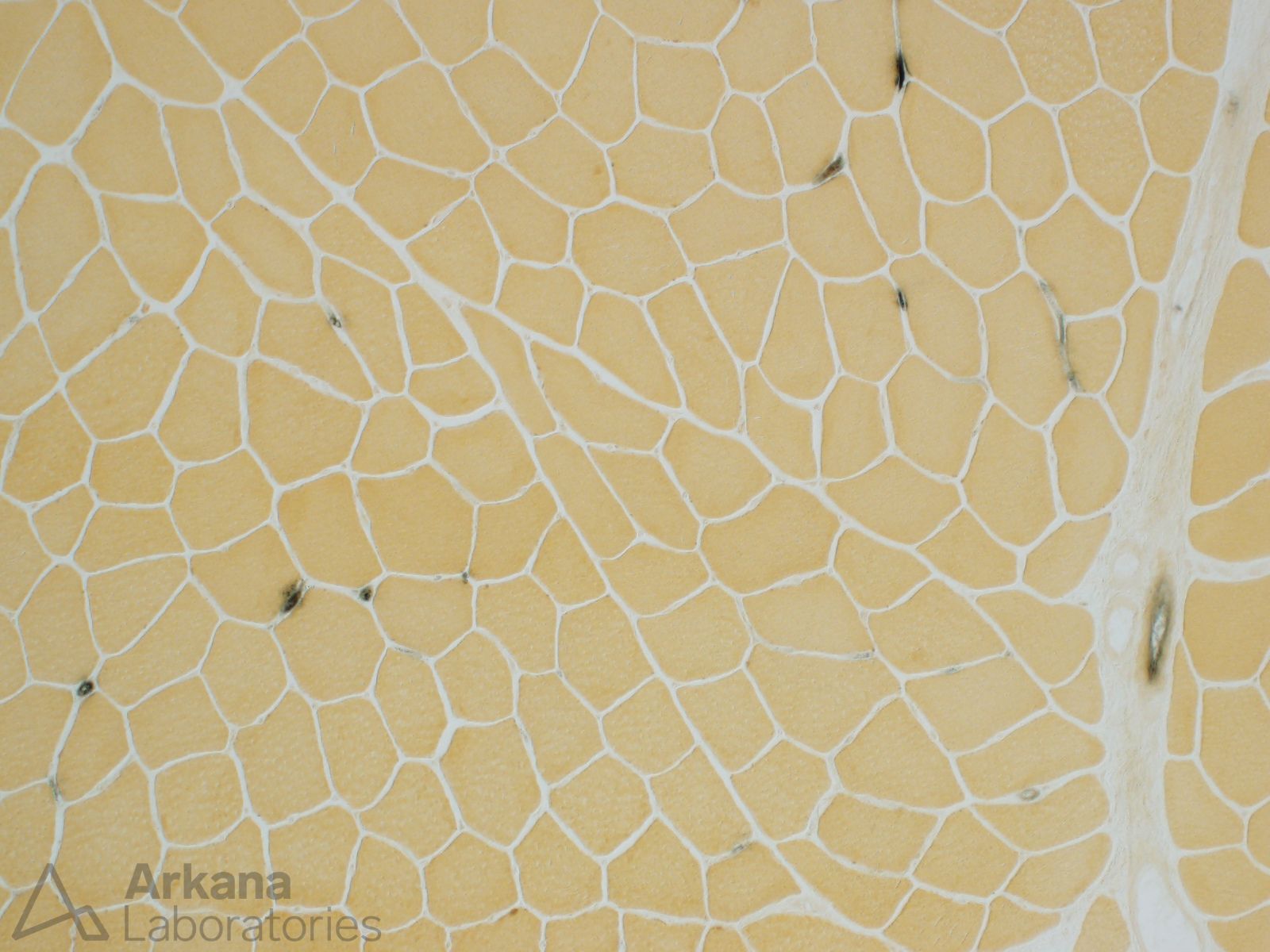
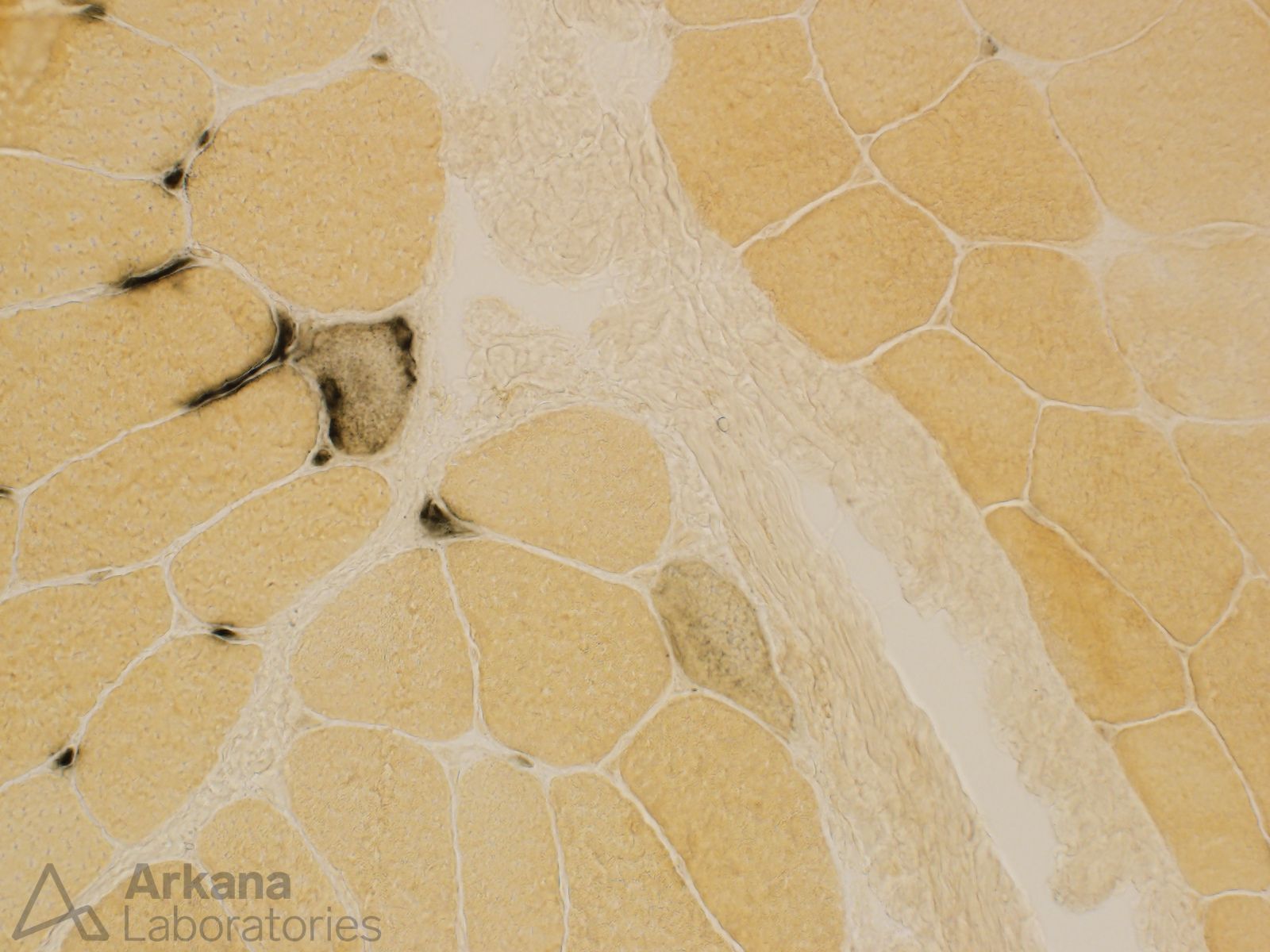
For comparison, Image #2 shows what the alkaline phosphatase stain looks like on normal skeletal muscle; Image #3 shows a higher power view of capillary and myofiber staining by alkaline phosphatase in an active myopathy; and Image #4 shows mild increase in capillary staining which is a common normal finding in areas of muscle biopsy containing intramuscular nerve twigs.
Answer:
Alkaline phosphatase is useful for highlighting damaged myofibers, capillaries and perimysium. In this case, note that the damaged myofibers are present in a somewhat patchy distribution and show a predilection to be perifascicular in location. Also note the increase staining of perimysium and capillaries.
A perifascicular distribution of muscle fiber injury may be seen in the setting of dermatomyositis and anti-synthetase syndrome. Myositis specific autoantibody panel testing is useful for resolving this pathologic differential diagnosis. Immunohistochemical stains for MxA (a marker for dermatomyositis) and HLA DR (a marker for anti-Synthetase syndrome) performed on the muscle biopsy tissue are also of utility in further evaluating this case.
Reference(s) / Additional Reading:
- Nix JS, Moore SA. What Every Neuropathologist Needs to Know: The Muscle Biopsy. J Neuropathol Exp Neurol. 2020 Jul 1;79(7):719-733. doi: 10.1093/jnen/nlaa046. Erratum in: J Neuropathol Exp Neurol. 2021 Mar 22;80(4):387. doi: 10.1093/jnen/nlaa096. PMID: 32529201; PMCID: PMC7304986.
- Palterer B, Vitiello G, Carraresi A, Giudizi MG, Cammelli D, Parronchi P. Bench to bedside review of myositis autoantibodies. Clin Mol Allergy. 2018 Mar 7;16:5. doi: 10.1186/s12948-018-0084-9. PMID: 29540998; PMCID: PMC5840827.
- Mariampillai K, Granger B, Amelin D, Guiguet M, Hachulla E, Maurier F, Meyer A, Tohmé A, Charuel JL, Musset L, Allenbach Y, Benveniste O. Development of a New Classification System for Idiopathic Inflammatory Myopathies Based on Clinical Manifestations and Myositis-Specific Autoantibodies. JAMA Neurol. 2018 Dec 1;75(12):1528-1537. doi: 10.1001/jamaneurol.2018.2598. PMID: 30208379; PMCID: PMC6583199.
- Conticini E, Dourado E, Bottazzi F, Cardelli C, Bruno L, Schmidt J, Carli L, Cavagna L, Barsotti S. Idiopathic inflammatory myopathies: one year in review 2023. Clin Exp Rheumatol. 2024 Feb;42(2):213-224. doi: 10.55563/clinexprheumatol/dh5o6c. Epub 2024 Mar 14. PMID: 38488099.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.