This 26-year-old patient complained of progressive weakness and frequent falls over the past several years. On physical examination, the patient was noted to have upper extremity proximal and distal muscle weakness, bilateral lower extremity contractures with upgoing Babinski reflex bilaterally, and weakness of dorsiflexion and plantarflexion. Muscle biopsy was performed to evaluate for possible causes of the patient’s weakness, including myopathy.
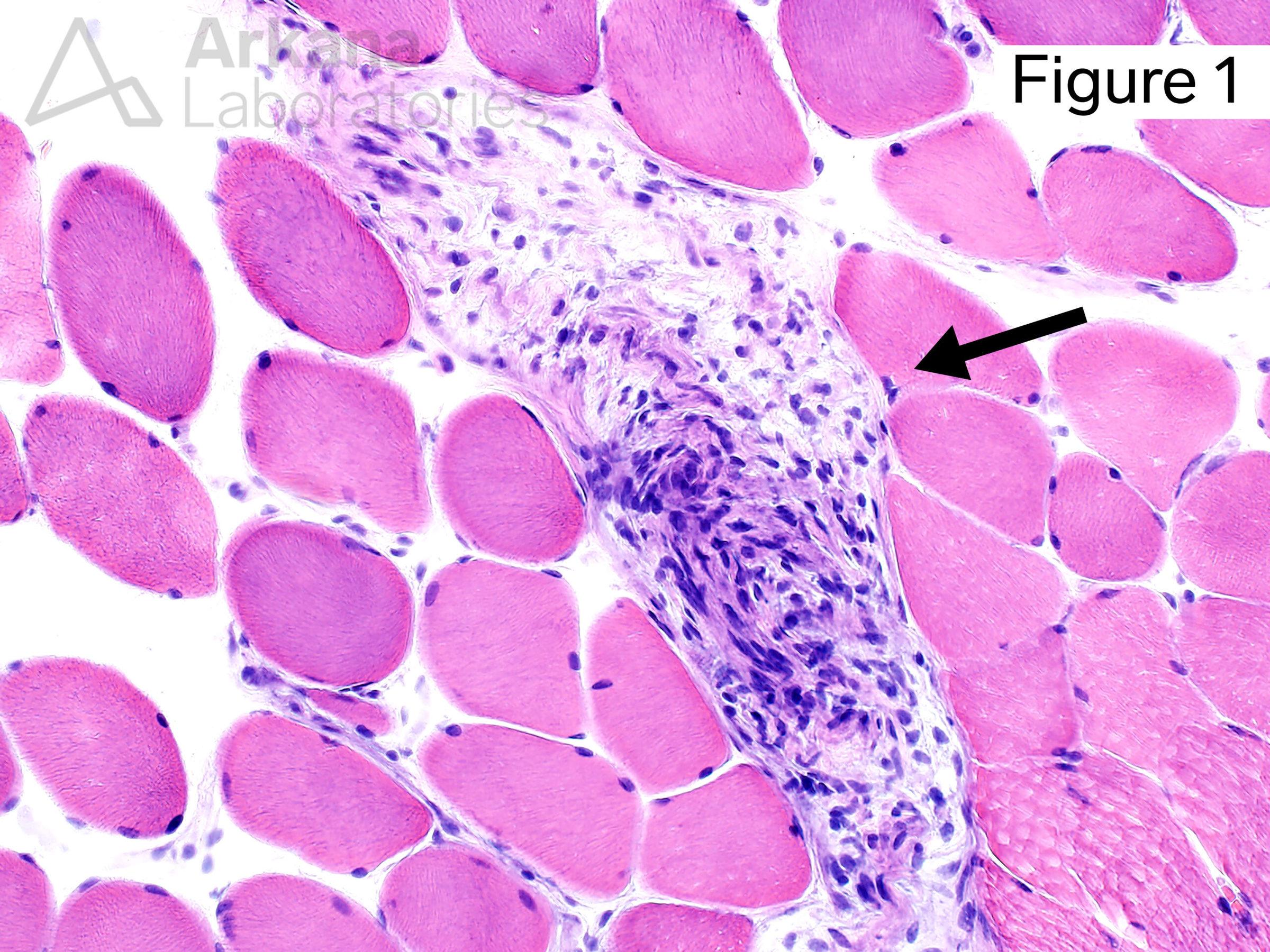
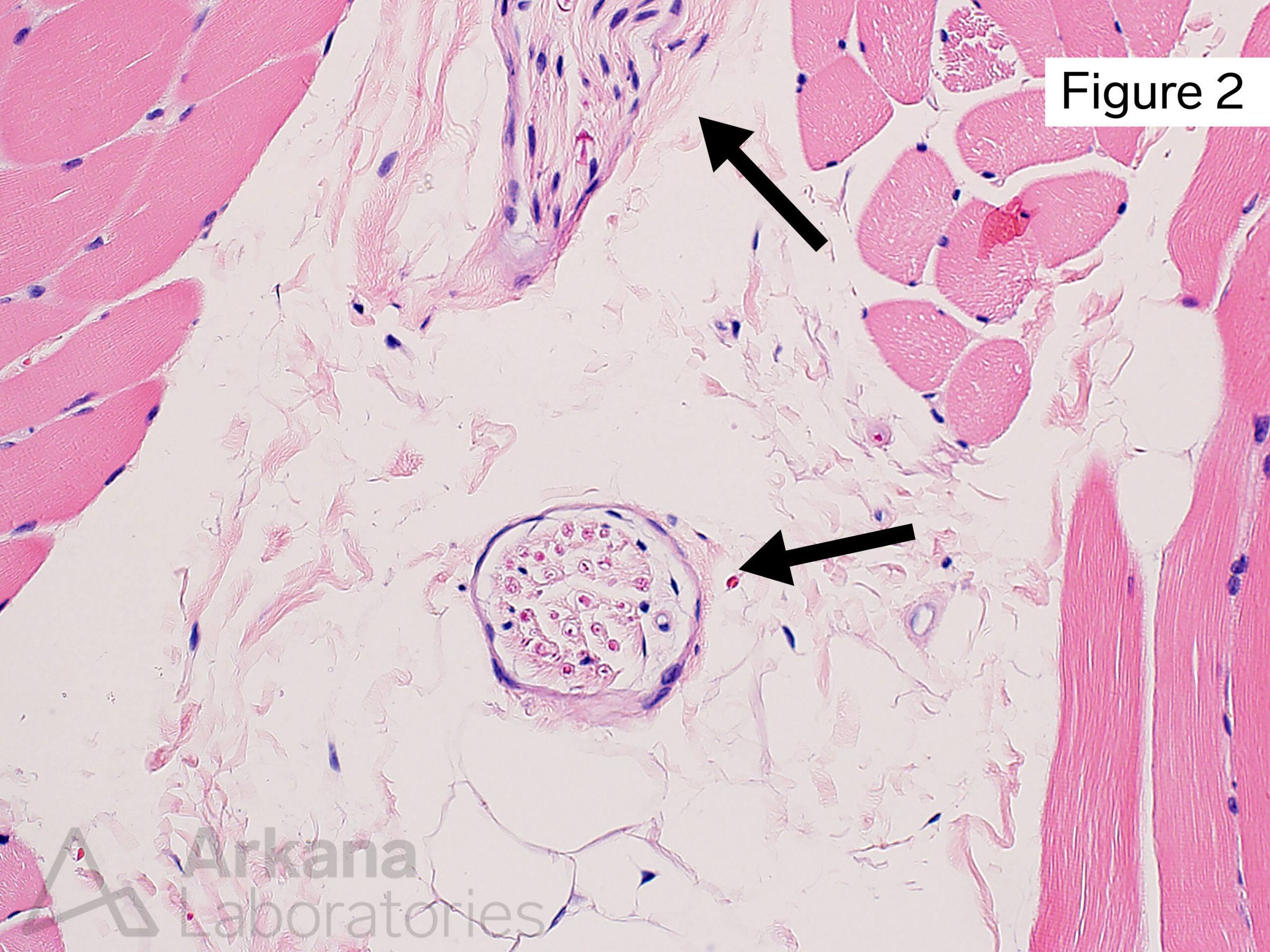
Based on the “incidental” biopsy finding demonstrated in Image #1 (see image #2 for normal comparison), what disease has been withheld from this patient’s prior clinical history?
A. Sarcoidosis
B. Amyloidosis
C. Lupus
D. Neurofibromatosis type 1
Answer: Neurofibromatosis type 1
The image demonstrates the presence of a variably cellular, disorganized appearing proliferation of bland appearing spindle cells within a small nerve twig. The less cellular areas have been described as having a “shredded carrots”-type appearance (Pathologists love to describe things as resembling food!!! … think “currant jelly” and “chicken fat” of post-mortem blood settling within the heart).
The morphologic appearance is consistent with the presence of a small intraneural neurofibroma within this patient’s muscle biopsy and correlates with the patient’s clinical history of Neurofibromatosis Type 1 / von Recklinghausen disease (D). This disease is caused by pathogenic mutations involving the NF1 gene (Chr 17q11.2) which encodes the neurofibromin 1 gene. The disease follows autosomal dominant inheritance, but a significant proportion of patients have no prior family history of the disease (i.e. de novo mutation).
Why were the other answers wrong?
Sarcoidosis (A) shows tight well-formed collections of mononuclear and multinucleate histiocytes with variable associated chronic inflammation rather than the spindle cells as seen in this lesion.
Amyloidosis (B) typically shows variably abundant relatively homogenous eosinophilic material. Amyloid deposition may be associated with chronic inflammation, plasma cells, and/or granulomata.
Lupus (C) patients may develop inflammatory neuropathy and/or myositis as a component of their disease. The abnormal cells noted within the nerve in our patient’s case are spindle-shaped and do not appear inflammatory in nature.
References
Friedman JM. Neurofibromatosis 1. 1998 Oct 2 [updated 2019 Jun 6]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mirzaa G, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2021. PMID: 20301288.
Kresak JL, Walsh M. Neurofibromatosis: A Review of NF1, NF2, and Schwannomatosis. J Pediatr Genet. 2016 Jun;5(2):98-104. doi: 10.1055/s-0036-1579766. Epub 2016 Mar 9. PMID: 27617150; PMCID: PMC4918700.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.