Clinical History
This 60-year-old patient presented with complaints of proximal greater than distal muscle weakness. Laboratory studies showed normal CPK and negative myositis specific autoantibody panel. EMG showed myopathic features.
Question
Which of the following best describes the pathologic alterations shown in Figures #1 and #2?
A. Inflammatory myopathy
B. Inflammatory neuropathy
C. Neuromyositis
D. Normal muscle
Answer- Neuromyositis
The correct answer is C. Neuromyositis
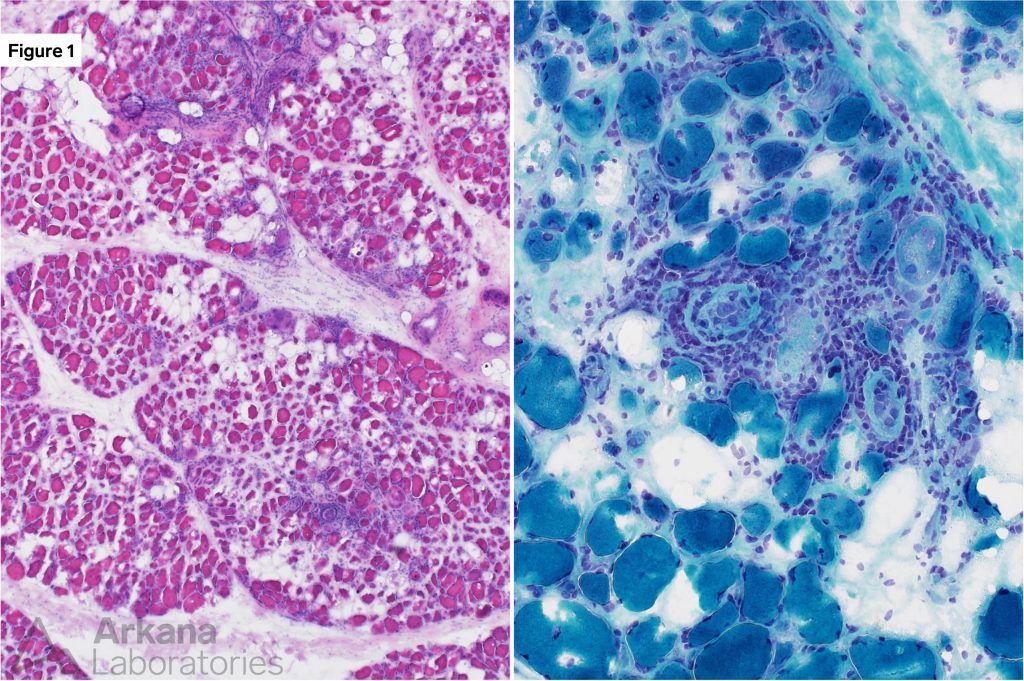
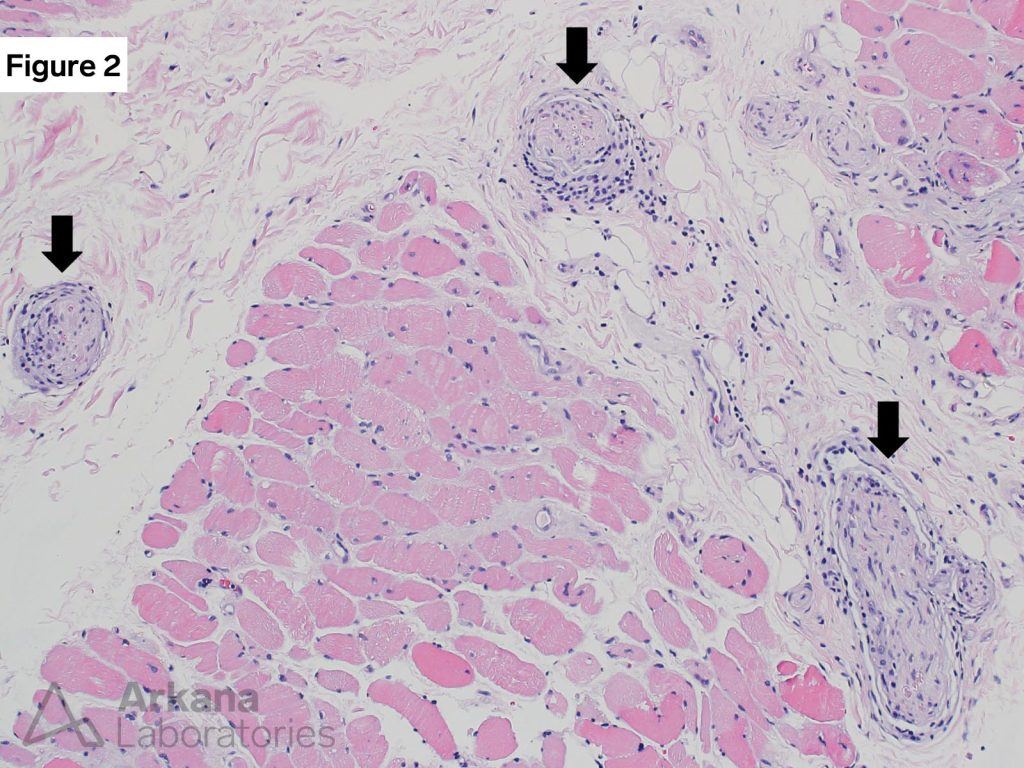
Figure 1: Frozen section H&E and modified Gomori Trichrome
These images show chronic inflammation within the endomysium and perimysium, variation in muscle fiber size, occasional regenerating and necrotic muscle fibers. These features are consistent with the presence of an acquired inflammatory myopathy.
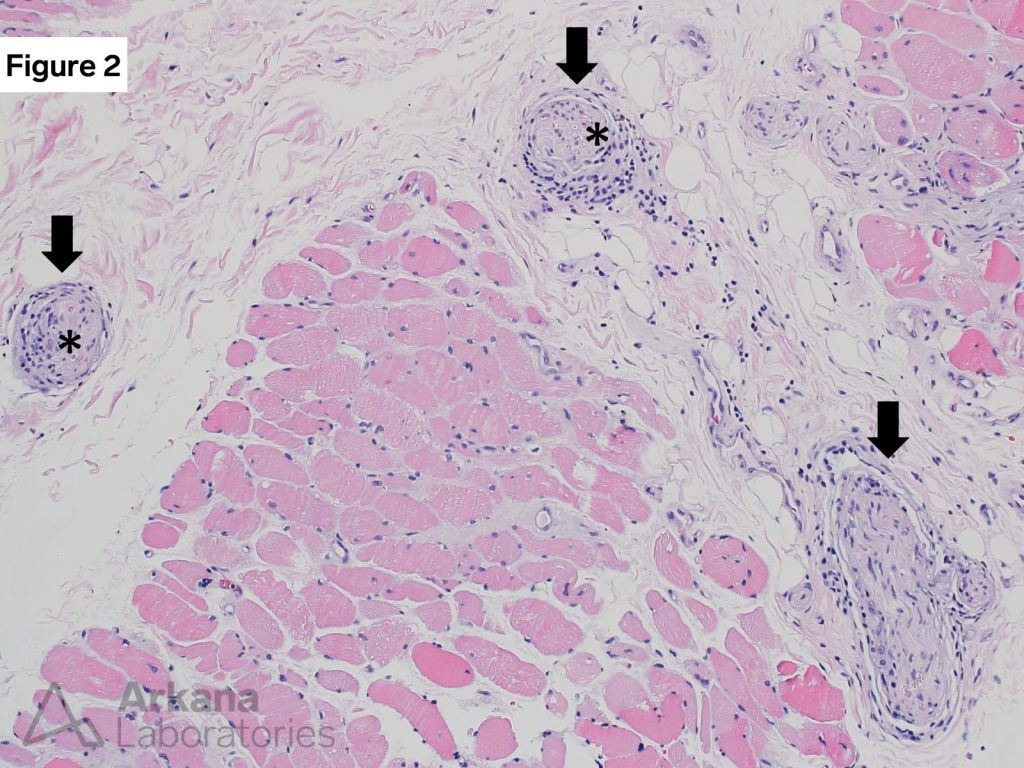
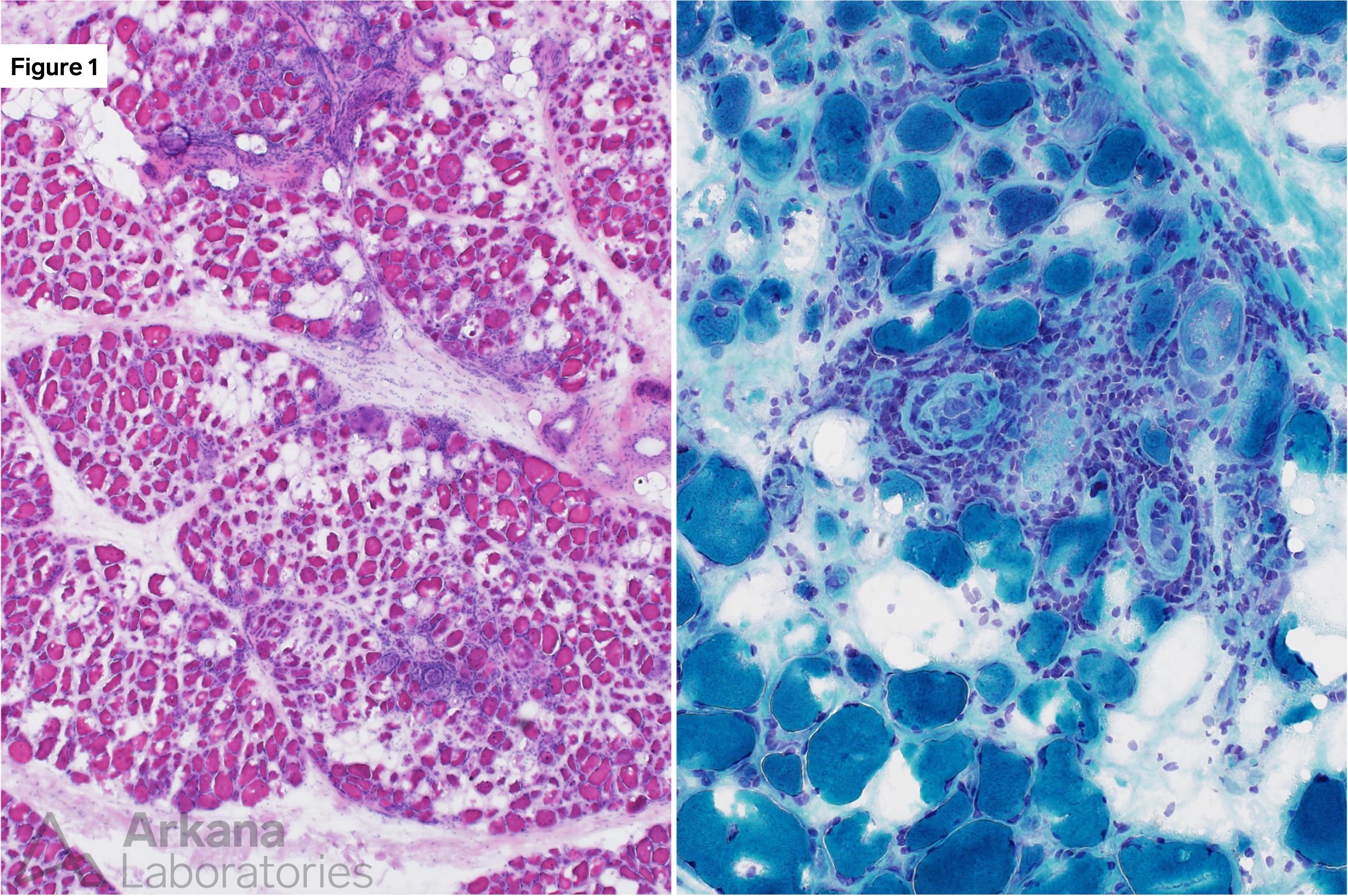
Figure 2: FFPE section H&E
Arrows show small nerve twigs included in the muscle biopsy tissue. Note the patchy presence of chronic inflammatory cells surrounding the nerve fascicles, as well as within the perineurium and endoneurium (asterisks).
Neuromyositis
- The figures show inflammation involving skeletal muscle and intramuscular peripheral nerve twigs. This is best categorized as “neuromyositis.” Features diagnostic for vasculitis were not seen.
- Concurrent inflammatory neuropathy and inflammatory myopathy is not common, and has been reported in association with dermatomyositis and polymyositis. MxA immunohistochemical stain (a marker of dermatomyositis) in this case was negative.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.