This 45-year-old previously healthy patient presented with a 4-year history of progressive numbness and dysesthesias involving their hands and feet which dramatically worsened over the past month. Family history was negative for neuromuscular disorder. Laboratory studies showed increased arsenic level, and normal vitamin B12, B6, and B1 levels. The patient did not take any medications.
Based on Figures #1 – #4, what test should be ordered to confirm the pathologic diagnosis for this patient’s neuropathy?
A. cANCA and pANCA
B. M. leprae PCR
C. T. pallidum IHC
D. ACE levels
Laboratory Testing:
- PCR on FFPE block tissue
- Positive for M. leprae
- Negative for M. lepromatosis
National Hansen’s Disease Program
9191 Interline Avenue
Baton Rouge, LA 70809
Phone: 225-756-3733
Fax: 225-756-3734
Website: https//www.hrsa.gov/hansens-disease/index.html
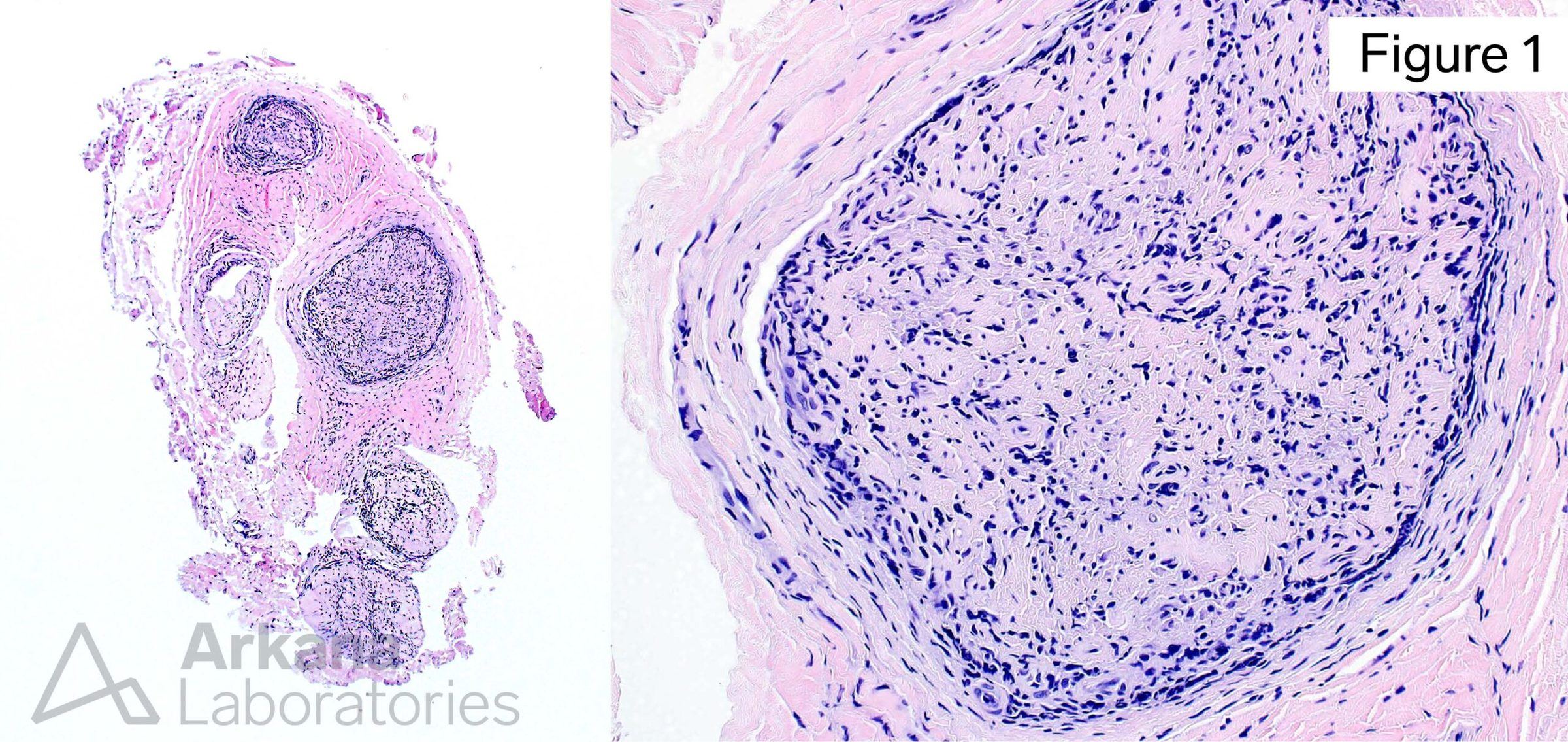
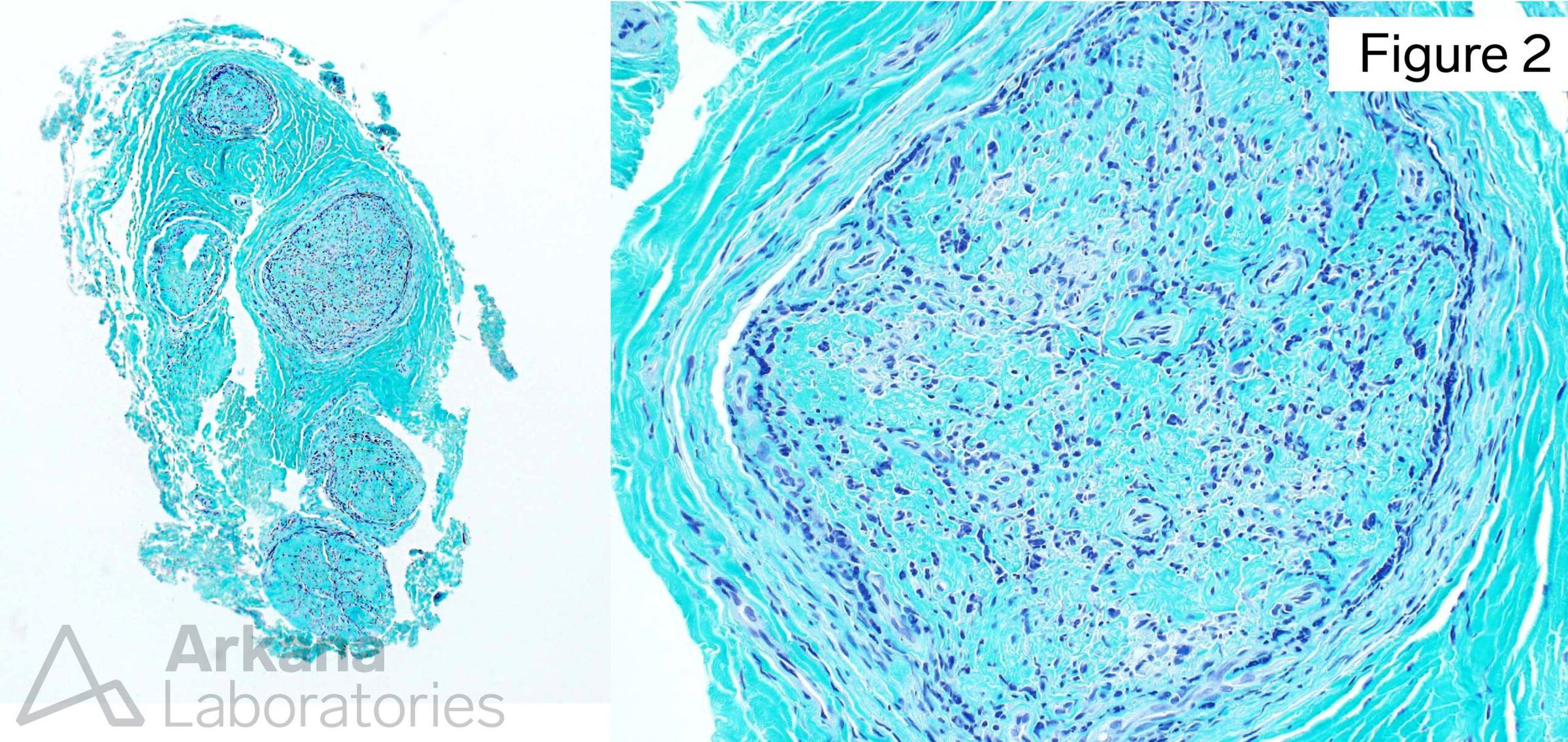
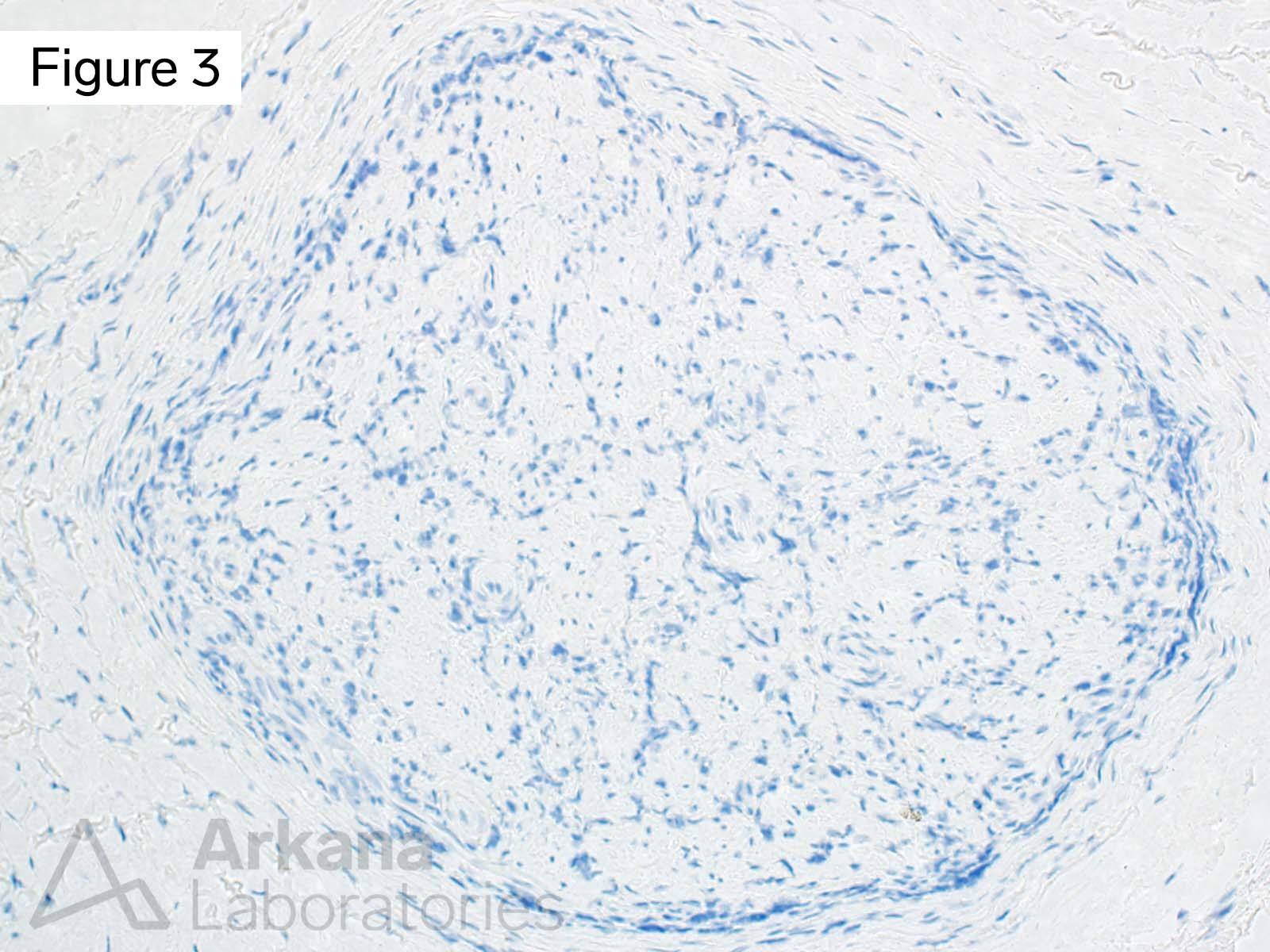
The images demonstrate the presence of an inflammatory neuropathy with complete loss of axons (end-stage nerve), and rare acid fast bacilli. Polymerase Chain Reaction (PCR) performed on paraffin block tissue detected the presence of Mycobacterium leprae DNA, and confirms the pathologic diagnosis of Leprous neuropathy (neuropathy related to Hansen’s disease).
The patient was started on treatment with Rifampin, Moxifloxacin, and Minocycline.
Answer: M. leprae PCR
Leprosy is a chronic mycobacterial infection affecting predominantly skin and peripheral nerves, but also eyes, oronasal mucosa, testicles, bones and other tissues. M. lepra (Hansen’s bacillus) and M. lepromatosis are obligate intracellular acid-fast Gram-positive pathogens with tropism for macrophages and Schwann cells. The bacterium grows best at 27-30oC and therefore is predisposed to infect cold areas of skin.
The bacillus does not grow in artificial media. Transmission is felt to occur via droplets of oronasal secretions from sneezing or coughing, or direct contact; human to human, and animal reservoir to human. Approximately 2/3rds of human infections in the Southern United States are related armadillo exposure.
The clinical and histologic spectrum of leprosy reflects the variability of host immune response:
- Tuberculoid: granulomatous response (epithelioid giant cells); limited organisms
- Dimorphous: borderline tending toward tuberculoid vs lepromatous
- Lepromatous: lack of granulomatous response; foamy macrophages heavily parasitized by freely multiplying organisms
References/Additional Reading
Oliveira IVPM, Deps PD, Antunes JMAP. Armadillos and leprosy: from infection to biological model. Rev Inst Med Trop Sao Paulo. 2019 Sep 12;61:e44. doi: 10.1590/S1678-9946201961044. Erratum in: Rev Inst Med Trop Sao Paulo. 2019 Nov 25;61:e44err. PMID: 31531622; PMCID: PMC6746198.
Salgado CG, Barreto JG. Images in clinical medicine. Leonine facies: lepromatous leprosy. N Engl J Med. 2012 Apr 12;366(15):1433. doi: 10.1056/NEJMicm1106238. PMID: 22494123.
Esfandbod M. Images in clinical medicine. Tuberculoid leprosy. N Engl J Med. 2011 Apr 28;364(17):1657. doi: 10.1056/NEJMicm1011992. PMID: 21524216.
Eichelmann K, González González SE, Salas-Alanis JC, Ocampo-Candiani J. Leprosy. An update: definition, pathogenesis, classification, diagnosis, and treatment. Actas Dermosifiliogr. 2013 Sep;104(7):554-63. doi: 10.1016/j.adengl.2012.03.028. Epub 2013 Jul 17. PMID: 23870850.
https://en.wikipedia.org/wiki/Mycobacterium_leprae
https://www.nps.gov/kala/learn/historyculture/damien.htm
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.