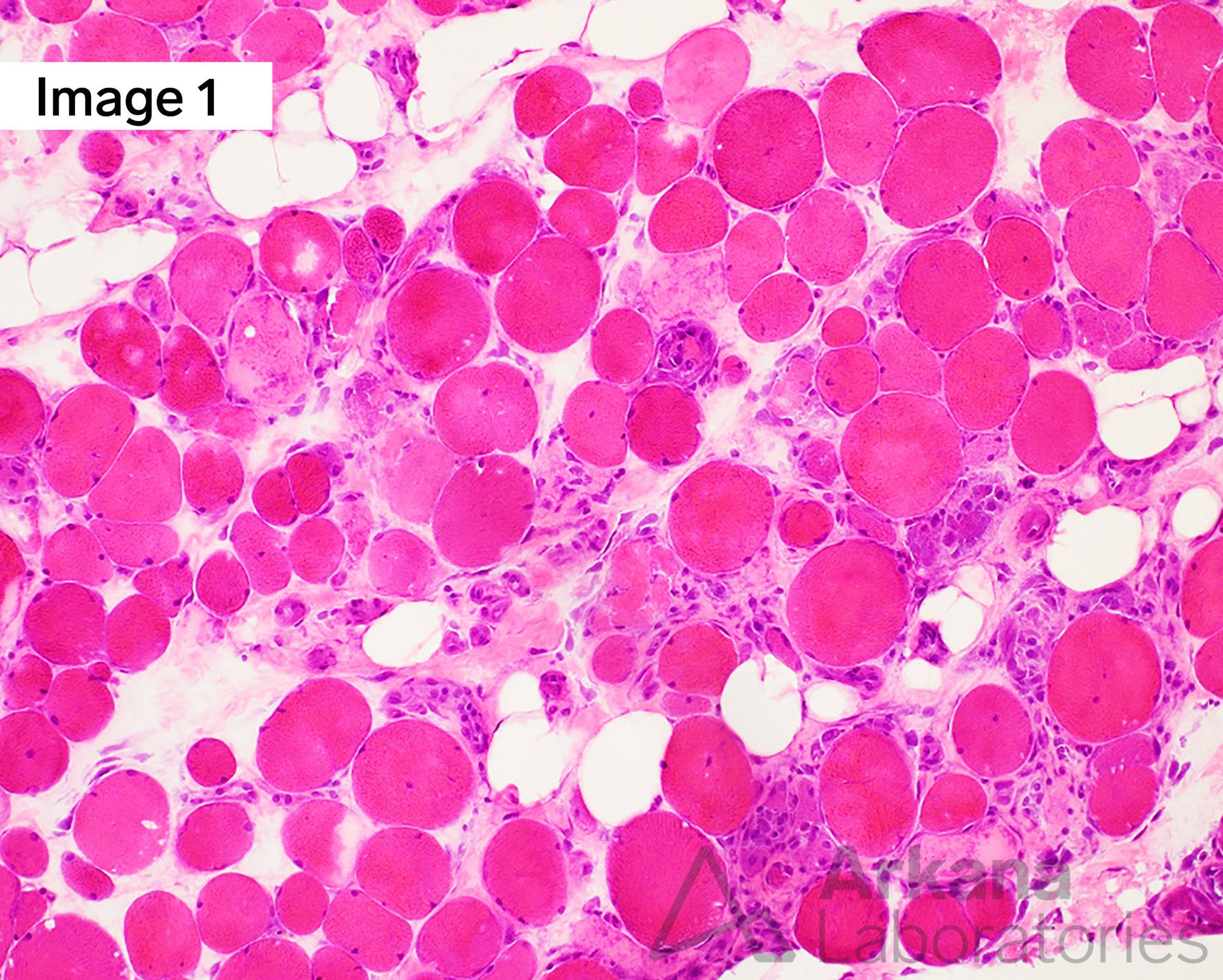
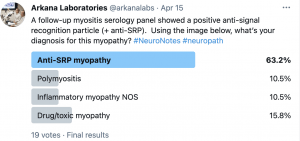
The patient is an 80-year-old female who presents with chief complaint of progressive proximal muscle weakness and carries a clinical diagnosis of polymyositis for nearly two decades. She was placed on a maintenance dose of steroids and was lost to follow-up for several years. No statin medication is reported. She was recently admitted after a wellness check revealed that she was unable to ambulate independently. CPK values ranged from 1500-7700. A skeletal muscle biopsy of the left thigh was performed. A follow-up myositis serology panel showed a positive anti-signal recognition particle (+ anti-SRP). Using the images, what’s your diagnosis for this myopathy?
Answer: Anti-SRP myopathy
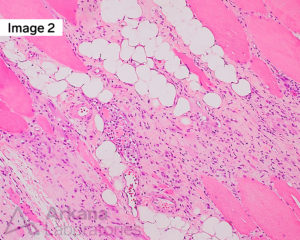
The skeletal muscle biopsy shows a spectrum of morphologic changes that range from active to chronic. The acute features show an active myopathic process characterized by marked variation in muscle fiber size with frequent regenerating and necrotic muscle fibers with sparse chronic inflammation (so-called “necrotizing myopathy”, a nonspecific pattern of muscle fiber injury). The features of chronicity are identified by muscle fibers with increased internalized nuclei, split fibers, fatty replacement, and fibrosis. An untreated inflammatory myopathy may lead to an end-stage muscle with fibroadipose tissue and essentially complete loss of viable muscle fibers. See references to learn more.
Why were the other answers wrong?
The muscle biopsy shows features of an immune-mediate necrotizing myopathy (IMNM). While steroid medication could significantly decrease the degree of chronic lymphocytic inflammation, only active myophagocytosis is seen, not lymphocytes infiltrating intact muscle fibers with associated muscle fiber injury, as would be seen in Polymyositis.
The morphologic features are those of necrotizing myopathy. Rendering a diagnosis of Inflammatory Myopathy, not otherwise specified (NOS), may mislead the clinician. This descriptive diagnosis is better suited for more challenging cases that do not neatly fit into the classic diagnostic rubric (i.e. not quite polymyositis, not quite dermatomyositis).
Drug/toxic myopath, is a good thought, especially as a necrotizing myopathy injury pattern may be seen in statin-related myopathy. However, no statin medication or other myotoxic medication/substance is reported in this case.
References:
Pinal-Fernandez I, et al. Immune-mediated necrotizing myopathy. Curr Rheumatol Rep. 2018; 26;20(4):21. PMID: 29582188.
Pinal-Fernandez I, et al. Longitudinal course of disease in a large cohort of myositis patients with autoantibodies recognizing the signal recognition particle. Arthritis Care Res. 2017;69:263-270. PMID: 27111848.
Suzuki S, et al. Inflammatory myopathy with anti-signal recognition particle antibodies: case series of 100 patients. Orphanet J Rare Dis. 2015 May 13;10:61. PMID: 25963141.
Watanabe Y, et al. Clinical features and prognosis in anti-SRP and anti-HMGCR necrotising myopathy. J Neurol Neurosurg Psychiatry. 2016 Oct;87(10):1038-44. PMID: 27147697.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.