Clinical History
This 30-year-old patient presented with complaints of severe exertional muscle stiffness and pain, and similar symptoms upon exposure to cold or hot temperatures. These symptoms had been present since they were a child. Family history was negative for neuromuscular disorder. CPK levels were within normal range. However, past medical history was significant for a prior episode of elevated CPK (~1000 range). The patient was not being treated with myotoxic medication or steroid.
Based on the clinical history and biopsy findings, genetic testing (sequencing panel) was suggested.
Question
Which of the following best characterizes features seen in figures #1 to #3?
A. Dermatomyositis
B. Vasculitis
C. Nonspecific changes
D. Necrotizing myopathy
Answer
The answer is C. Nonspecific changes.
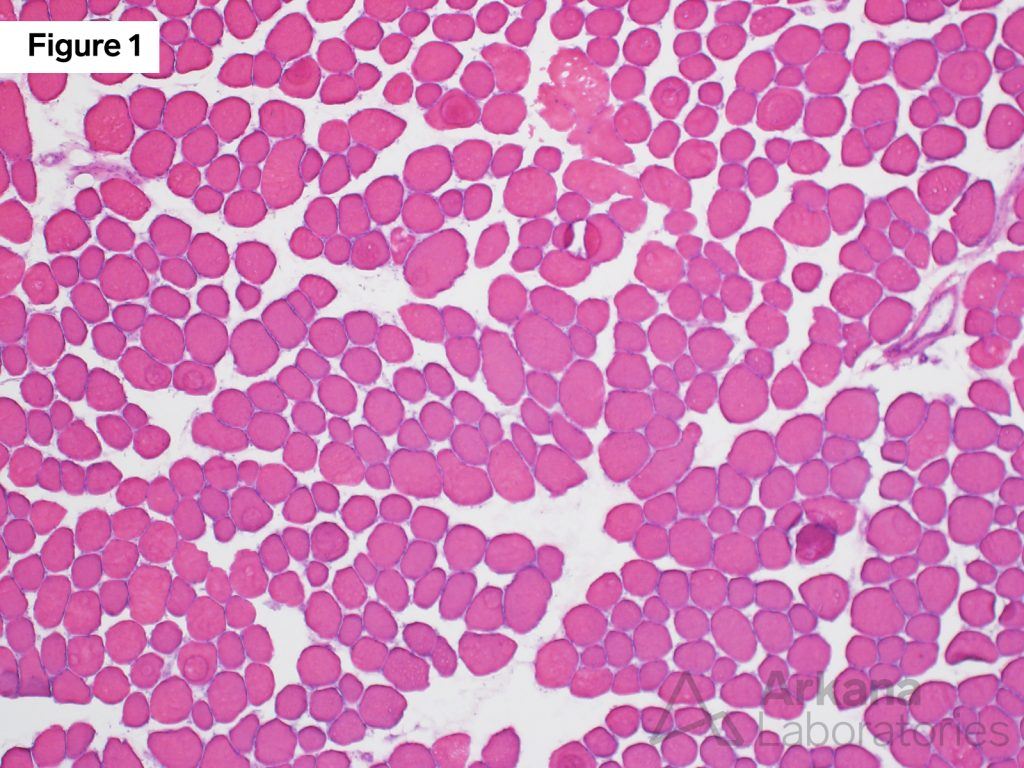
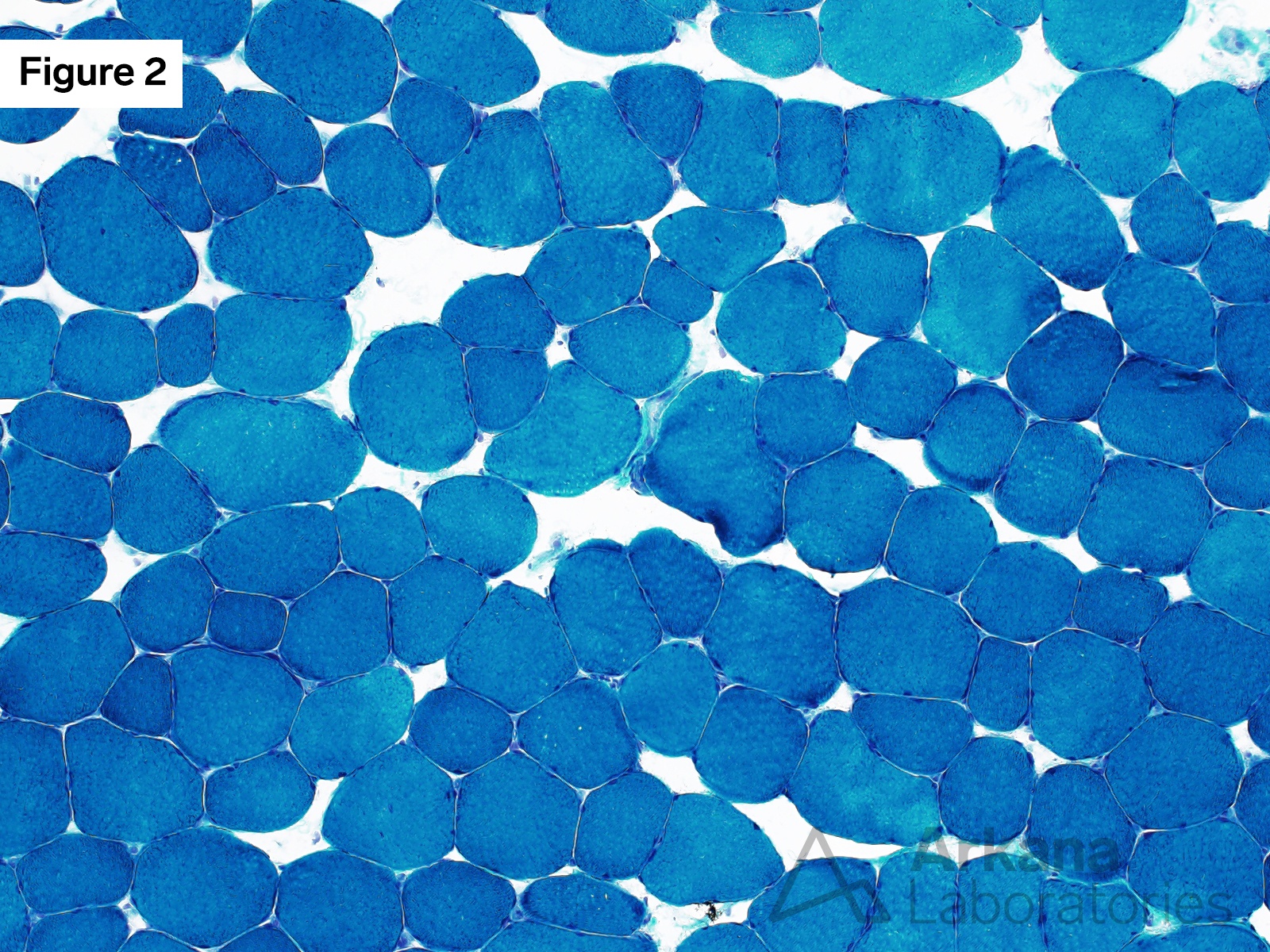
Figure 1: Hematoxylin and eosin stain
This medium low power magnification image shows mild variation in muscle fiber least mean diameter. No necrotic or regenerating muscle fibers are seen, no inflammation is seen, and no increase in the number of internalized nuclei is noted. The optically clear areas between muscle fibers represents artifact due to issue edema.

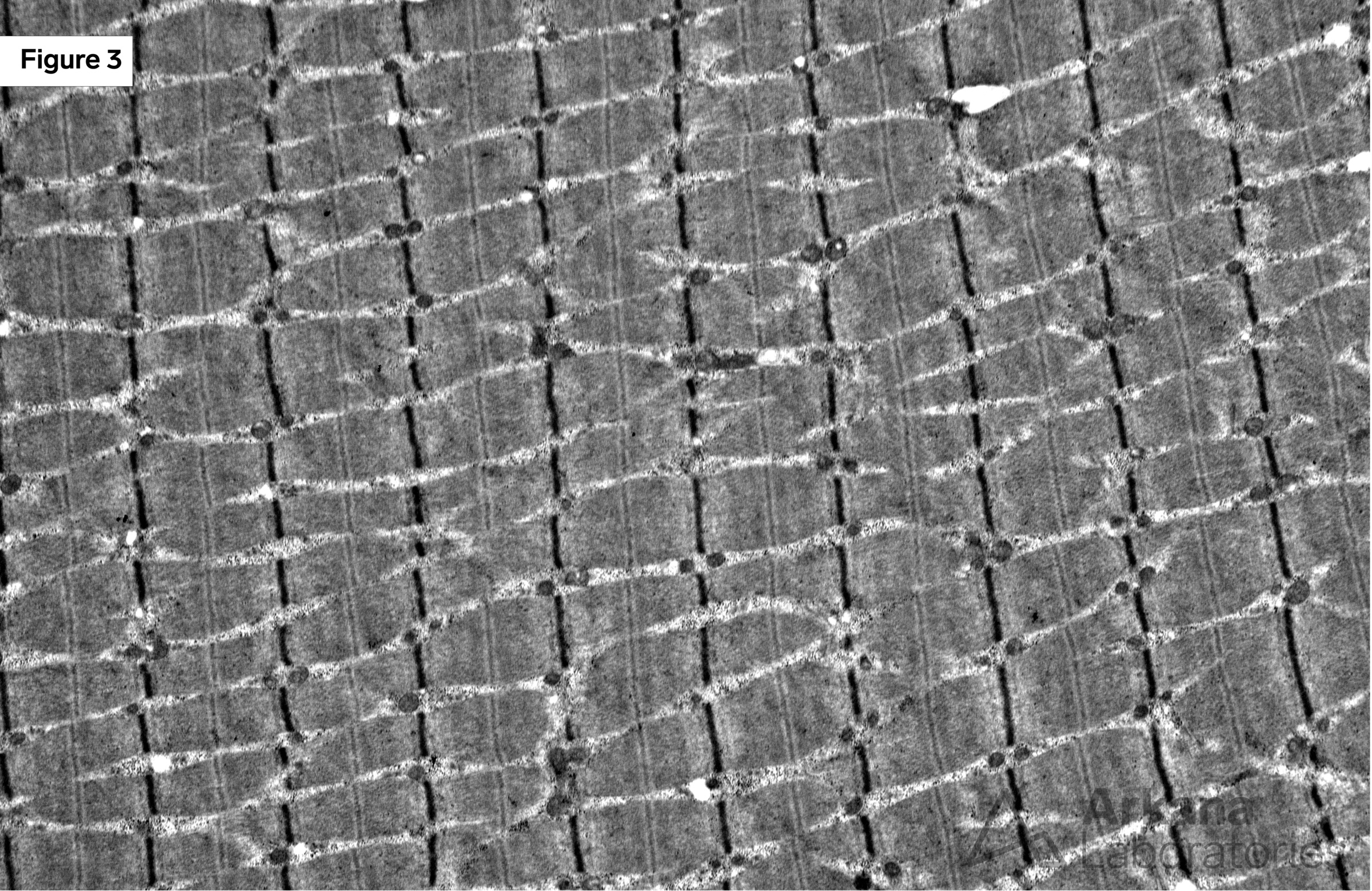
Figure 2: Modified Gomori Trichrome stain
This medium power magnification image features similar to that demonstrated on the hematoxylin and eosin stained section. Once again, mild variation in muscle fiber size is noted.
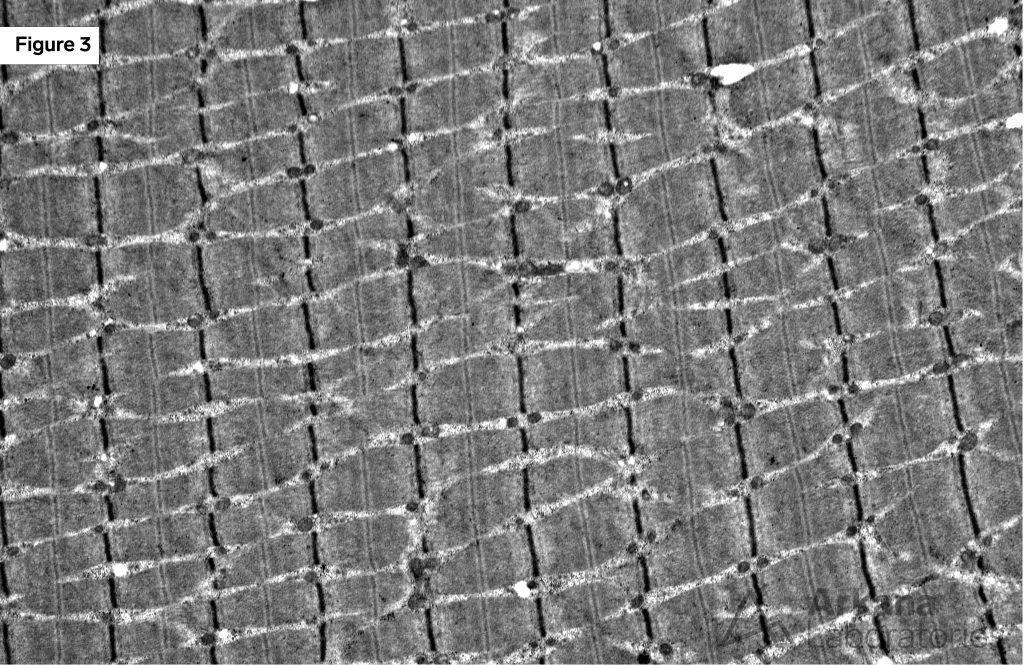
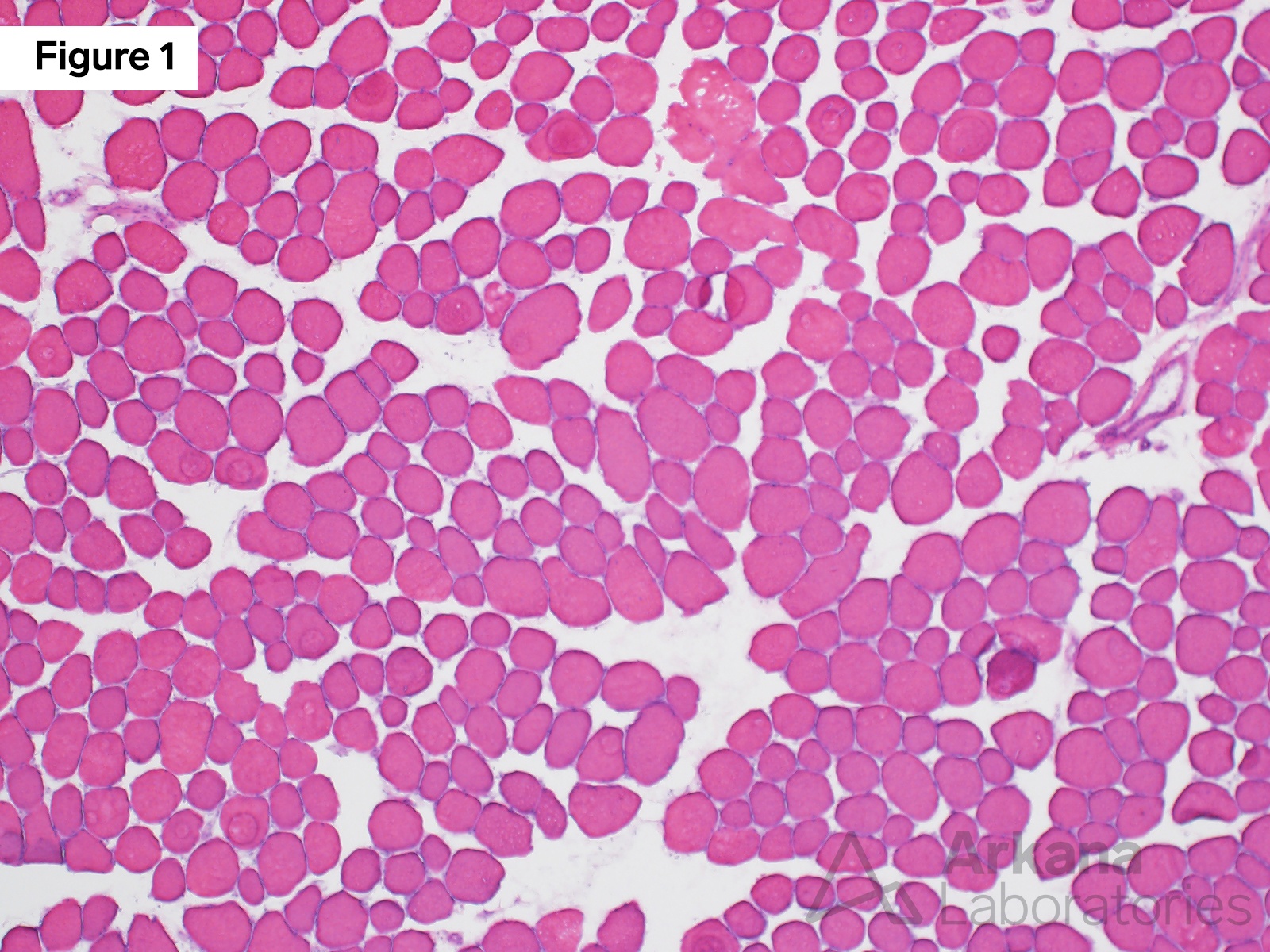
Figure 3: Electron microscopy
Electron microscopy showed normal appearing muscle.
Nonspecific Changes
- The morphologic features are mild in degree and not specific as to etiology. In essence, pathologic alterations to explain the patient’s signs and symptoms are not seen in the biopsy tissue.
- Genetic testing subsequently detected a heterozygous Pathogenic variant involving the CLCN1 gene (encodes chloride voltage-gated channel 1). The specific variant had been previously reported in patients with autosomal dominant myotonia congenita (Thomsen disease).
Reference(s) / Additional Reading
- Matthews E, Holmes S, Fialho D. Skeletal muscle channelopathies: a guide to diagnosis and management. Pract Neurol. 2021 Jun;21(3):196-204. doi: 10.1136/practneurol-2020-002576. Epub 2021 Feb 9. PMID: 33563766.
- Stunnenberg BC, LoRusso S, Arnold WD, BarohnRJ, Cannon SC, Fontaine B, Griggs RC, Hanna MG, Matthews E, Meola G, Sansone VA, Trivedi JR, van Engelen BGM, Vicart S, Statland JM. Guidelines on clinical presentation and management of nondystrophic myotonias. Muscle Nerve. 2020 Oct;62(4):430-444. doi: 10.1002/mus.26887. Epub2020 May 27. PMID: 32270509; PMCID: PMC8117169.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.