Clinical History
This 40-year-old female patient presented with a three month of bilateral medial thigh pain and edema. Her past medical history was significant for type 2 diabetes, end-stage renal disease (ESRD) due to diabetic nephropathy with associated secondary hyperparathyroidism and diabetic heel ulcers. Laboratory studies show elevated ESR, normal/negative CPK, ANA and ANCA.
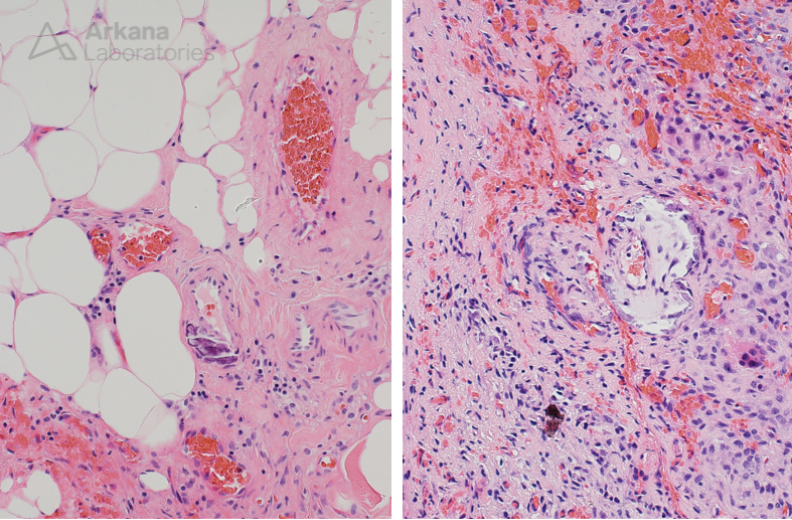
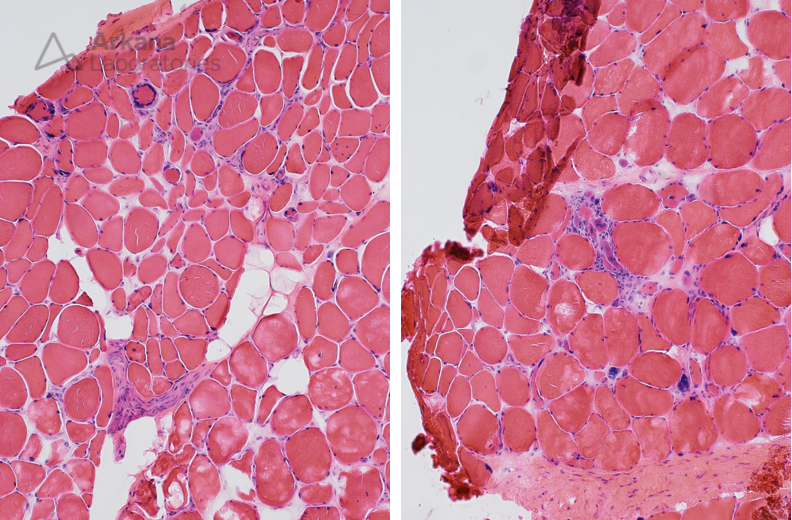
The patient’s muscle biopsy showed mild myopathic changes, with focal minimal chronic lymphoid inflammation, Type 2 muscle fiber atrophy, and neurogenic atrophy (chronic and active). Her muscle biopsy tissue included adjacent fibroadipose tissue.
The pathologic abnormalities seen in the fibroadipose tissue are consistent with which of the following?
A. Atherosclerosis
B. Calciphylaxis
C. Vasculitis
D. Eosinophilic fasciitis
Figure 1: Medium magnification image showing variation in muscle fiber size, mild myopathic changes, focal very mild chronic lymphoid inflammation. No micromineralization was seen within intramuscular blood vessels.
Figure 2: High magnification image showing two small arterioles with micromineralization of their walls. Associated fibrosis, fat necrosis and chronic inflammation was also present.
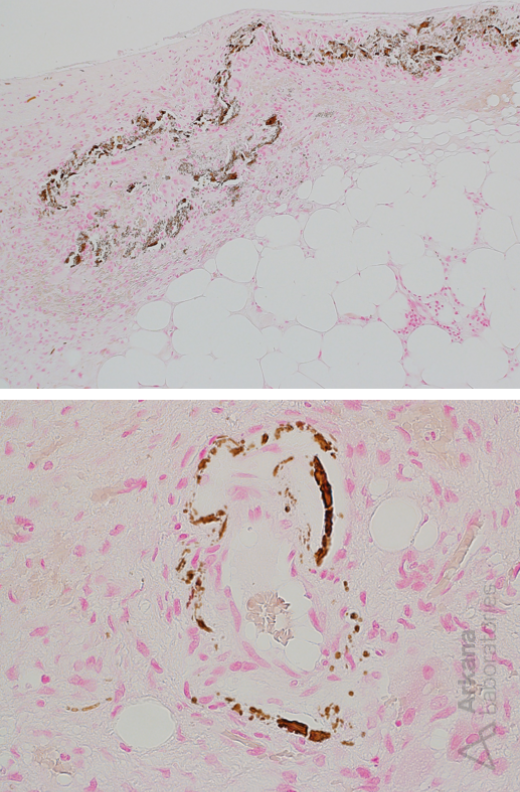
Figure 3: High magnification image showing positive dark brown to black staining of vascular micromineralization with von Kossa preparation.
The correct answer is B. Calciphylaxis
- AKA calcficic uremic arteriolopathy, calcifying panniculitis
- Relatively uncommon life threatening vasculopathy characterized by micromineralization (calcification) of arteriolar microvasculature and thrombosis, most commonly in the setting of ESRD with secondary hyperparathyroidism (compromised calcium and phosphate homeostasis)
- Uncertain pathogenesis
- Variably involves skin (painful and ulcerating), adipose and/or viscera
- High risk of mortality: 45 – 80% 1 year mortality rate
- Poor response to therapy
- Risk factors: female sex, obesity, diabetes, vitamin K antagonists and ESRD
References/additional readings
- Westphal SG, Plumb T. Calciphylaxis. 2023 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30085562. https://www.ncbi.nlm.nih.gov/books/NBK519020/
- Gallo Marin B, Aghagoli G, Hu SL, Massoud CM, Robinson-Bostom L. Calciphylaxis and Kidney Disease: A Review. Am J Kidney Dis. 2023 Feb;81(2):232-239. doi: 10.1053/j.ajkd.2022.06.011. Epub 2022 Aug 12. PMID: 35970430.
- Edelstein CL, Wickham MK, Kirby PA. Systemic calciphylaxis presenting as a painful, proximal myopathy. Postgrad Med J. 1992 Mar;68(797):209-11. doi: 10.1136/pgmj.68.797.209. PMID: 1589381; PMCID: PMC2399253.
- Aouizerate J, Valleyrie-Allanore L, Limal N, Ayache SS, Gherardi RK, Audard V, Jerôme Authier F. Ischemic myopathy revealing systemic calciphylaxis. Muscle Nerve. 2017 Sep;56(3):529-533. doi: 10.1002/mus.25505. Epub 2017 Apr 23. PMID: 27935078.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.