The above painting shows podocytes with foot processes extending along the glomerular basement membrane of neighboring capillary loops. Effacement of podocyte foot processes occurs in primary podocytopathies, including minimal change disease (see electron photomicrograph below).
Minimal Change Disease
Minimal change disease (MCD) is the most common etiology of idiopathic nephrotic syndrome in children and is the third most common cause in adults, after focal segmental glomerulosclerosis and membranous glomerulopathy. A majority of cases are “primary”, require no additional workup, and are due to a circulating permeability factor. Several possible secondary causes have also been identified. Although these are rare, these should be considered in patients with steroid resistance or an atypical clinical course. Secondary causes of minimal disease include autoimmune diseases, medications, cancers, infections, atopic reactions, and other etiologies.
Lupus podocytopathy is the most common autoimmune etiology of minimal change disease (Bomback 2016). It is seen in 1-2% of biopsies in patients with systemic lupus erythematosus. It’s diagnosed clinically by meeting clinical criteria for lupus (established by the American College of Rheumatology), the presence of nephrotic syndrome, and severe to global podocyte foot process effacement. It can be seen with negative immunofluorescence, or with mesangial immune deposition, which can be accompanied by mesangial proliferation on light microscopy (Bomback 2016). Therefore, it can be seen without a diagnosis of lupus nephritis, with minimal mesangial lupus nephritis (class I lupus nephritis), or with mesangial proliferative lupus nephritis (class II lupus nephritis). Other autoimmune diseases less commonly associated with podocytopathies include sclerosing cholangitis, myasthenia gravis, Guillain-Barre syndrome, and dermatitis herpetiformis (Glassock 2003).
Medications & Allergens
Medications can induce minimal change disease, which is often due to a hypersensitivity reaction to the drug rather than nephrotoxicity of the agent. MCD can resolve upon discontinuation of the drug, and re-emerge upon re-exposure. Drugs associated with MCD include non-steroidal anti-inflammatory drugs (NSAIDs, most common), antibiotics, lithium, interferon, methimazole, tamoxifen, enalapril, penicillamine, gold salts, and probenecid (Glassock 2003). Similarly, immunizations rarely induce minimal change disease by a delayed type hypersensitivity response. Many allergens have been associated with MCD, possibly due to a hypersensitivity mechanism that is IgE-mediated. These include dust, pollen, food allergens (pork, dairy), bee stings, or reactions to environmental agents (poison oak, poison ivy, etc). Allergen avoidance in these cases is associated with remission of minimal change disease.
Both solid organ malignancies and hematologic neoplasms have been associated with minimal change disease. A disease association can be established when eradication of the tumor leads to improvement of proteinuria, or when proteinuria recurs with tumor recurrence. Solid tumors associated with minimal change disease include carcinomas (lung, pancreatic, colon, urothelial, renal cell, and prostate), thymoma, mesothelioma, oncocytomas, and neurilemmoma. Hematologic neoplasms associated with MCD include Hodgkin lymphoma, non-Hodgkin lymphoma, mycosis fungoides, Waldenstrom’s macroglobulinemia, chordoma, lymphoid hamartoma, angiofollicular lymph node hyperplasia, and Kimura disease (Glassock 2003). MCD occurring with malignancies (either solid organ or hematologic) is a rare complication. A majority of cases of MCD have no associated neoplasia.
Infections are additional, rare potential secondary causes of minimal change disease. These include HIV, tuberculosis, syphilis, schistosomiasis, and hydatid disease due to echinococcal infection. An infectious etiology can be established when treatment of the underlying infection leads to resolution of proteinuria. While secondary etiologies of minimal disease overall are uncommon, they can be considered in cases of prolonged nephrotic syndrome, steroid resistance, or recurrent disease. In these cases, treatment of the underlying condition may be critical and lead to resolution of proteinuria.
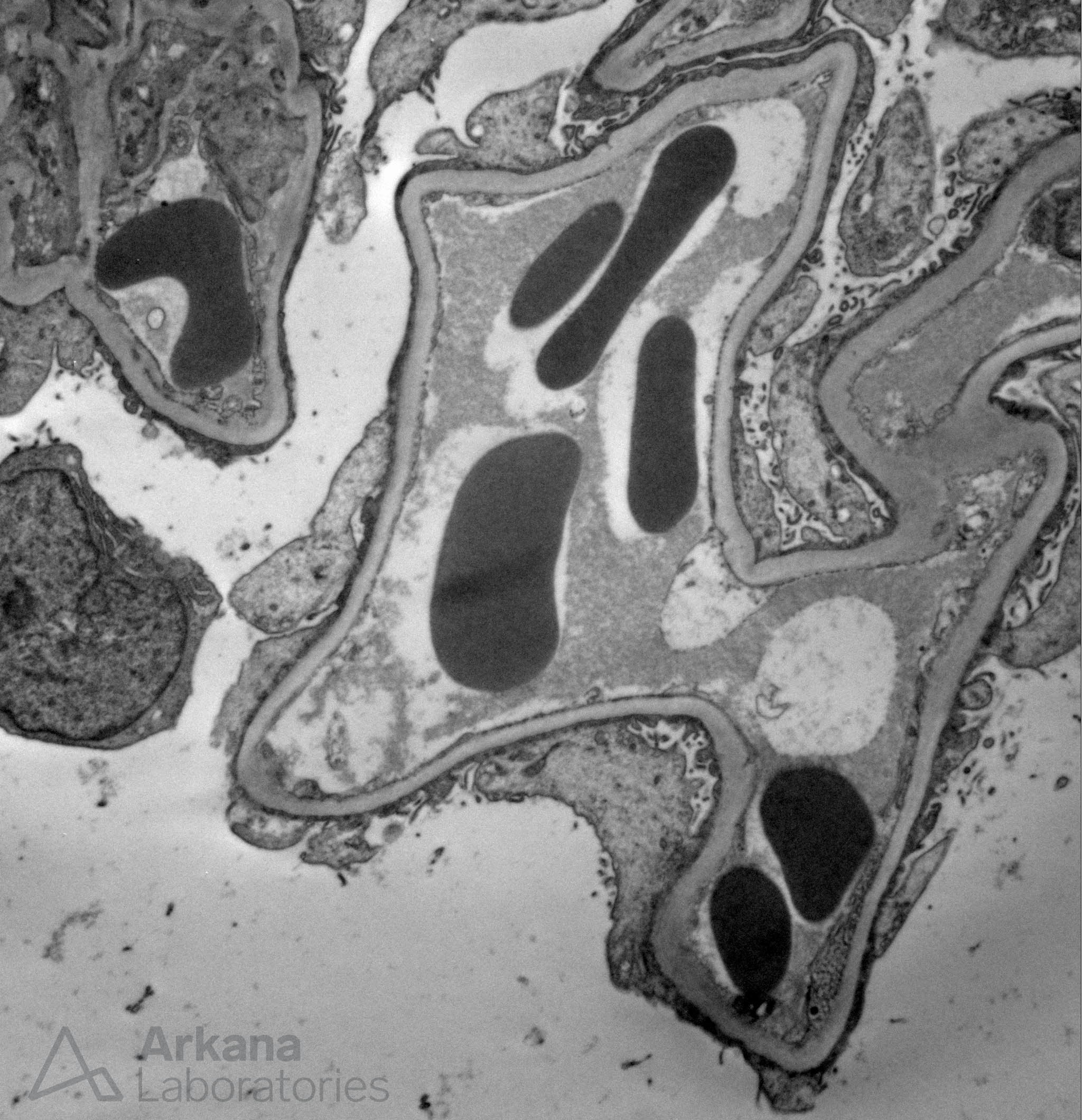
Podocyte foot process effacement in a case of minimal change disease.
References:
Bomback AS, Markowitz GS. Lupus podocytopathy: a distinct entity. Clin J Am Soc Nephrol 2016 Apr 7; 11 (4): 547-548.
Glassock RJ. Secondary minimal change disease. Nephrology Dialysis Transplantation 2003; 18 (6): vi52-vi58.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.


