Clinical History:
The patient is a 92-year-old-male and presented progressive muscle weakness that began in the left upper extremity and spread to the BLEs and bulbar muscles. CK WNL. EMG/NCS: widespread denervation and reinnervation.
Based on the images below, what is the most likely etiology?
Answer Choices:
A. Denervation and reinnervation
B. Myofibrillar myopathy
C. Sporadic inclusion body myositis (sIBM)
D. A and B
Answer:
Choice D: A and B, both denervation and reinnervation, and myofibrillar myopathy.
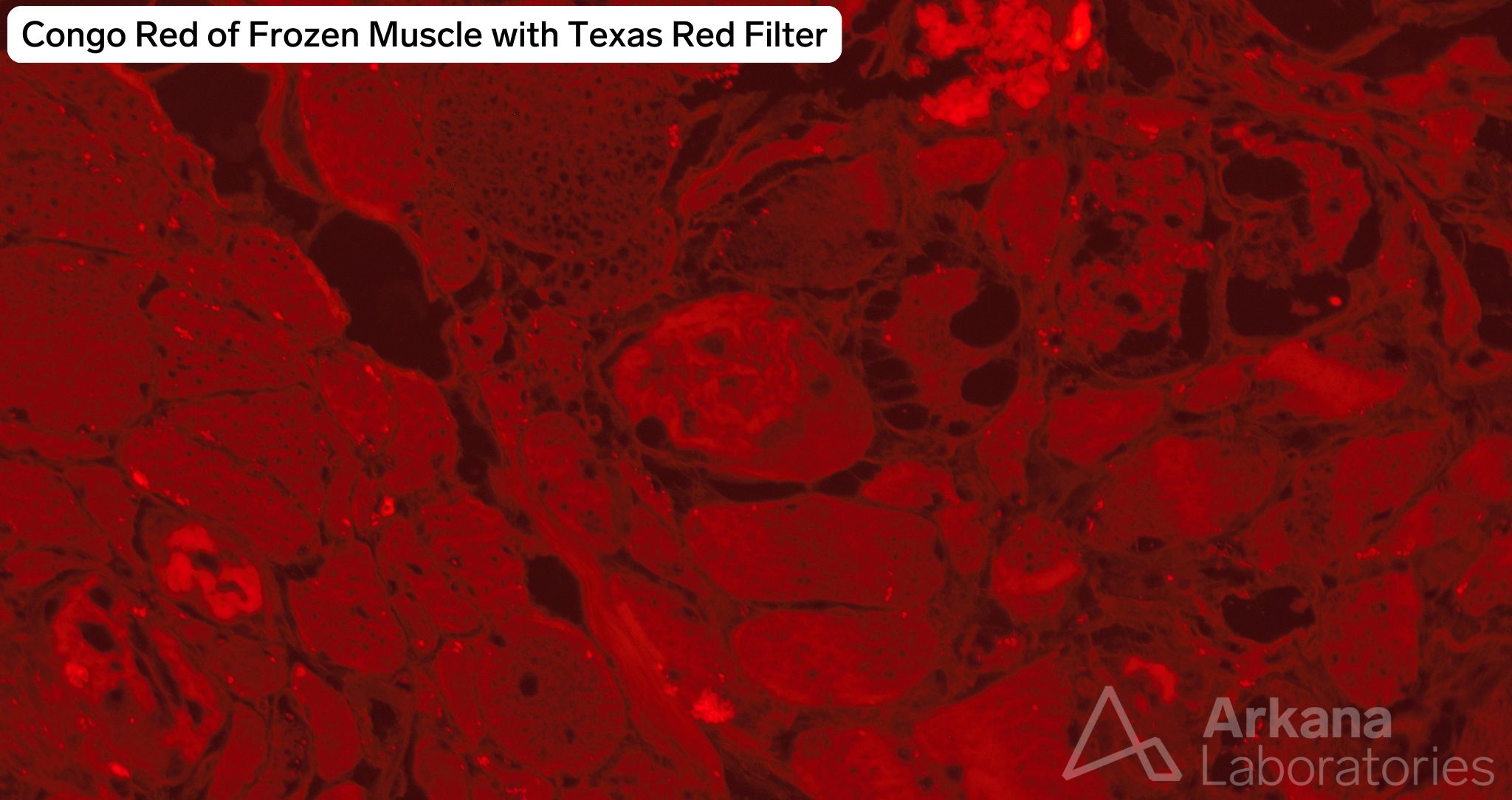
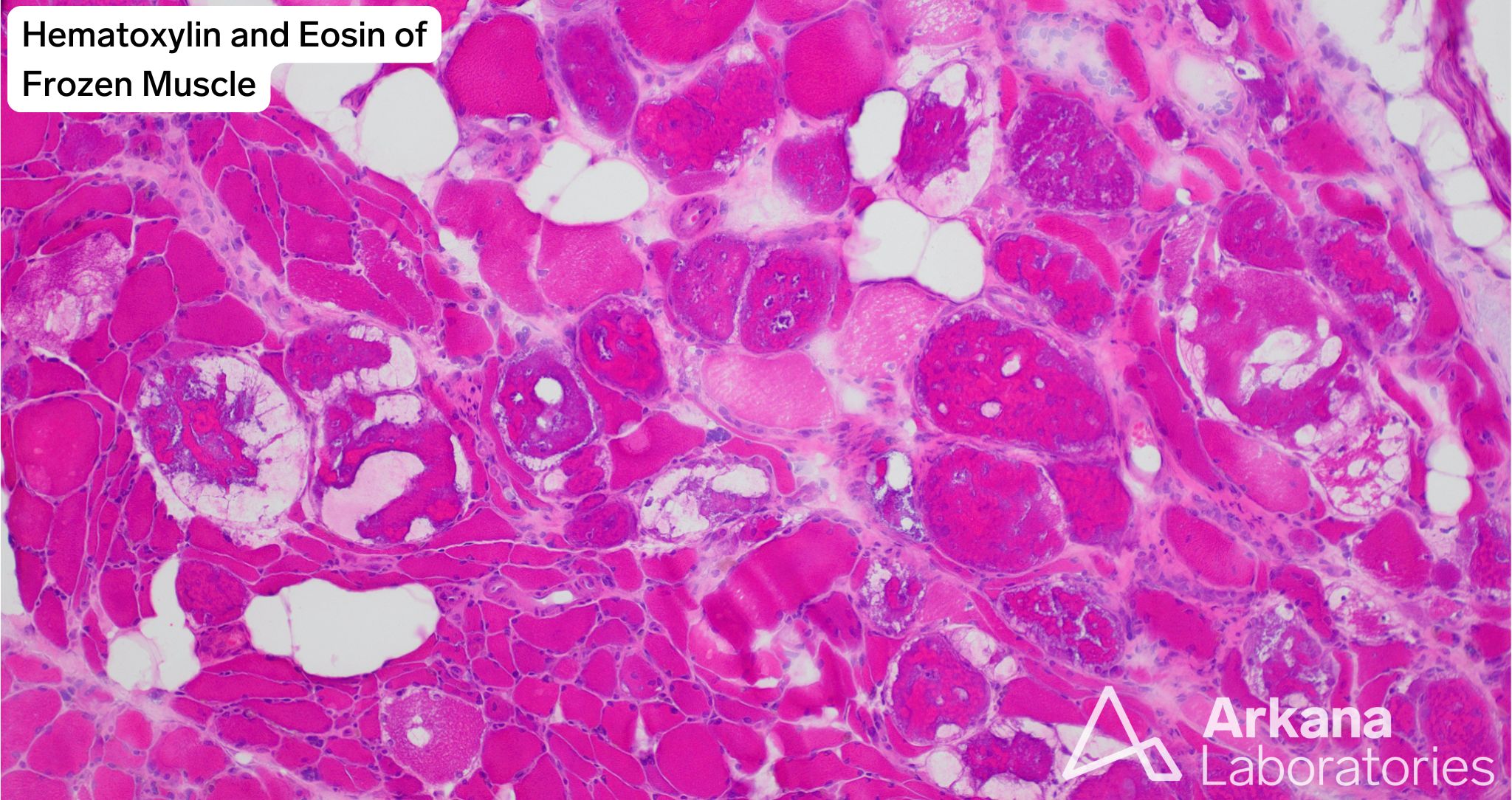
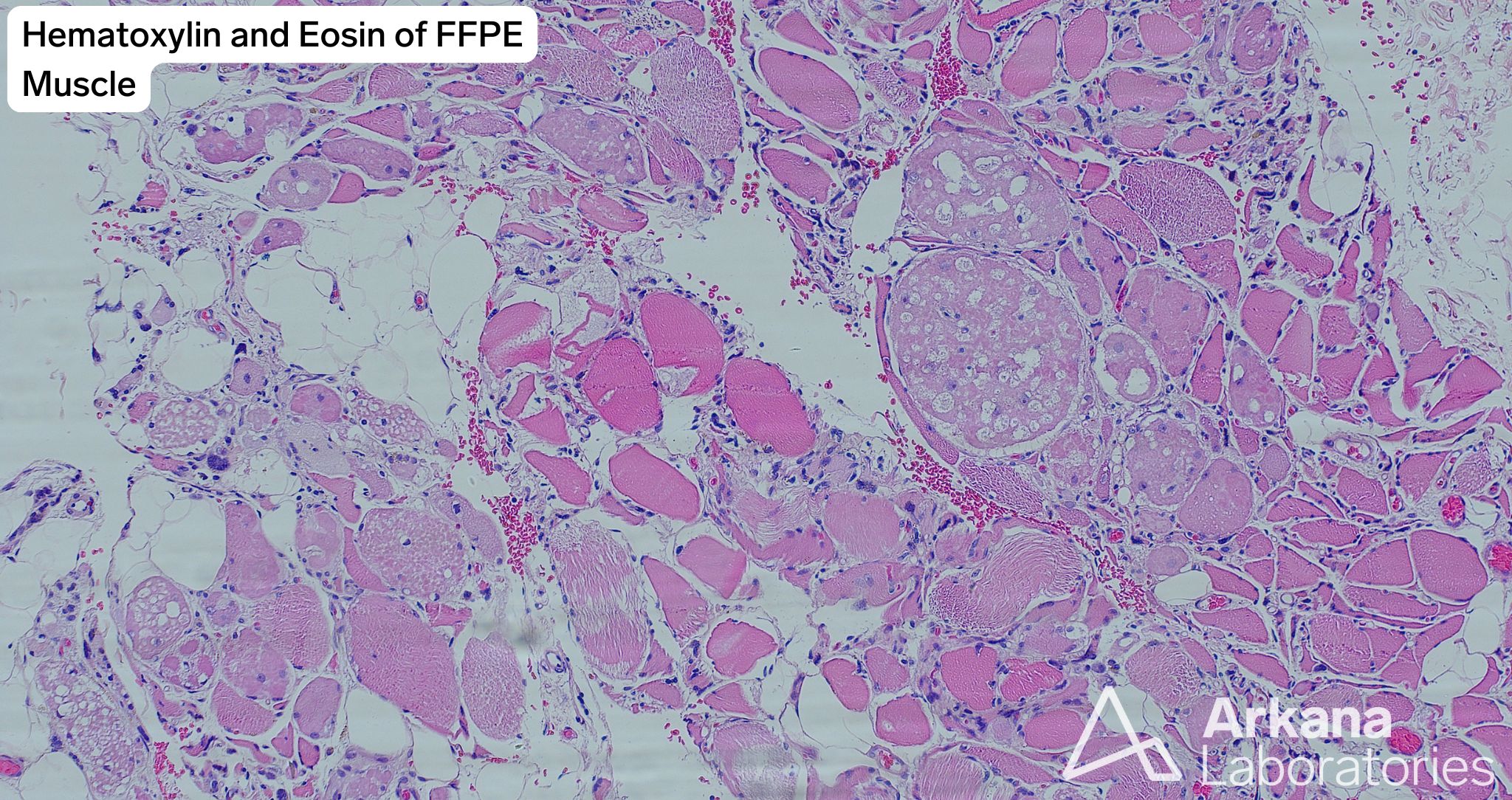
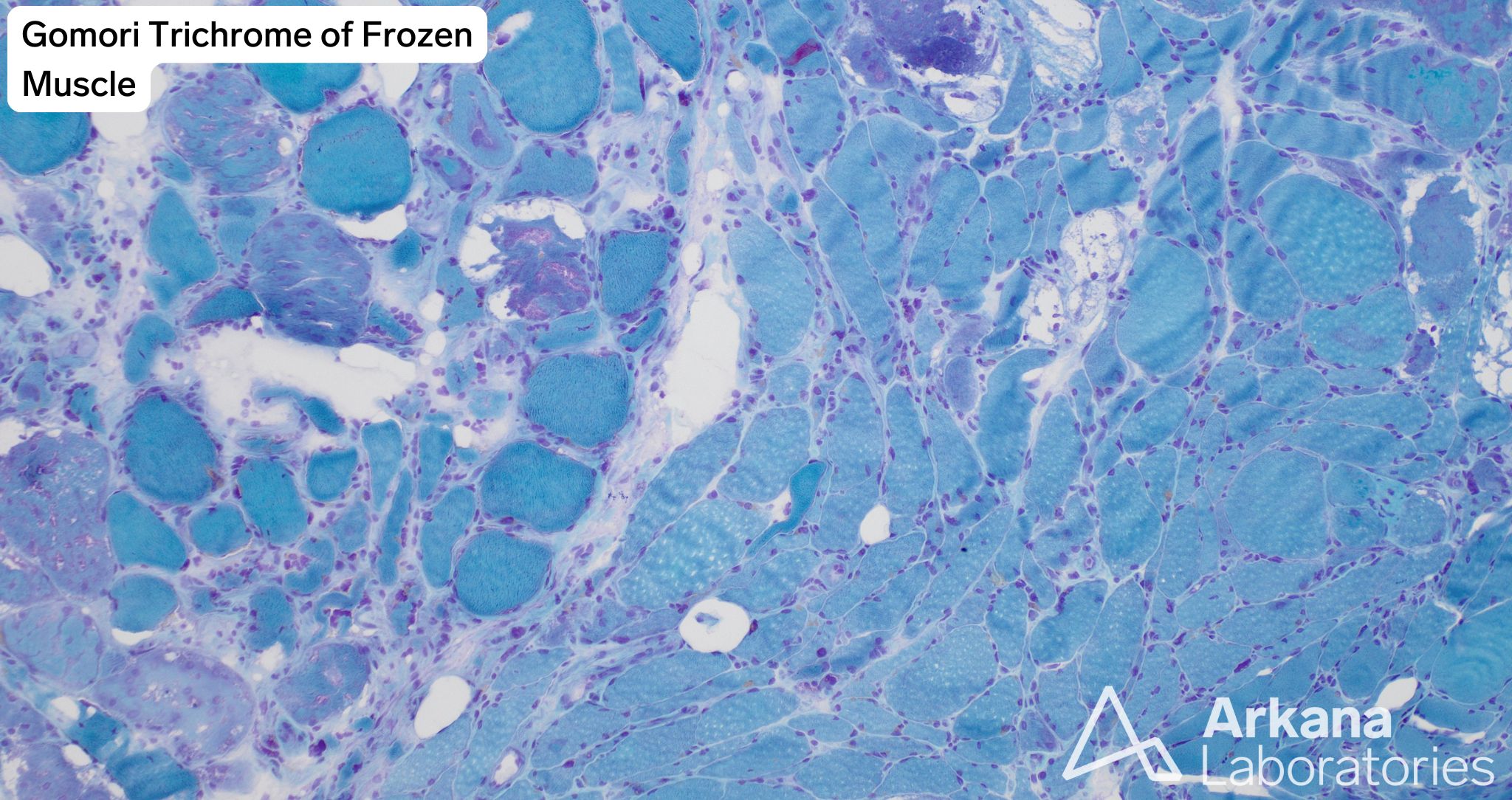
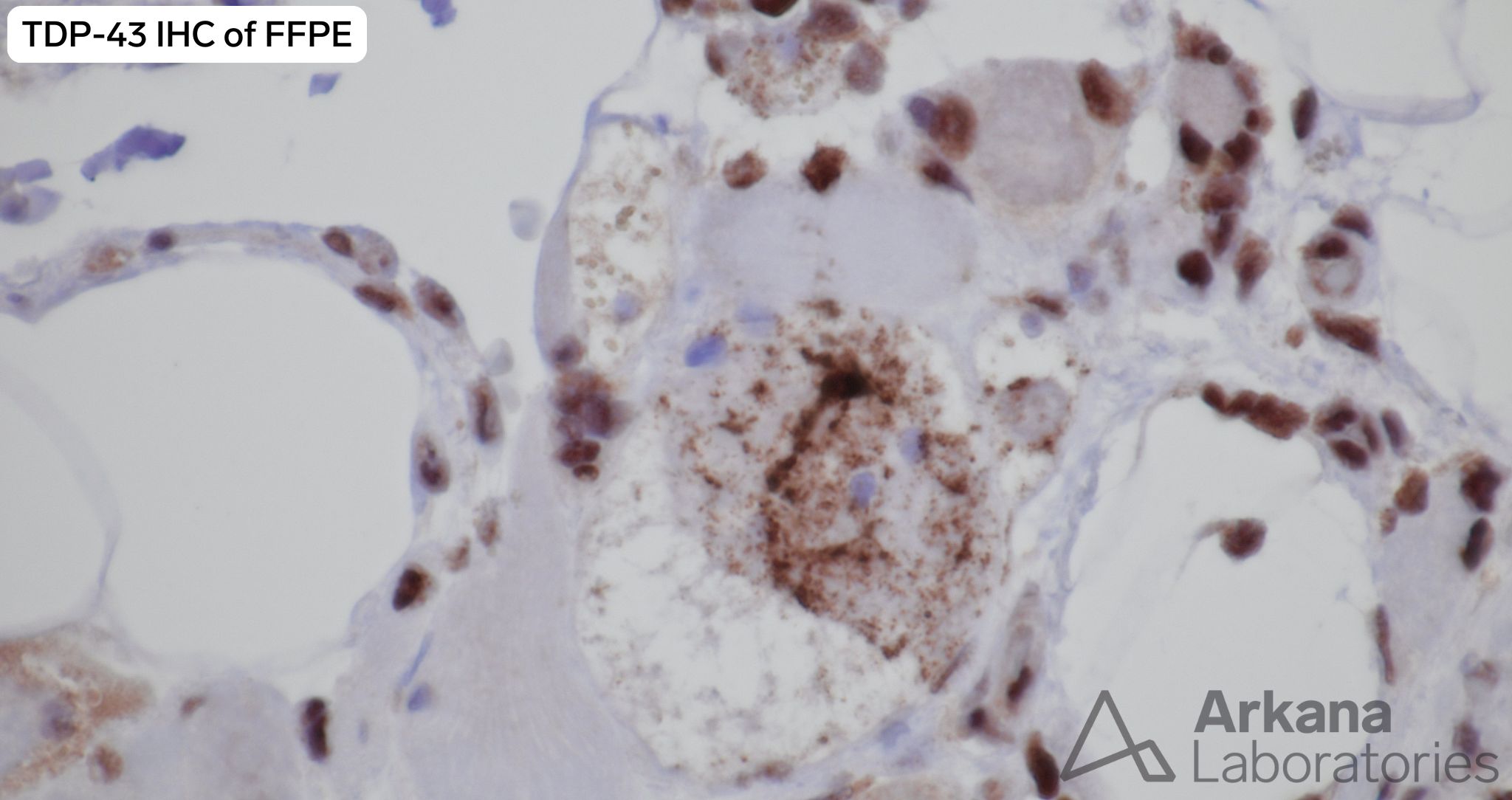
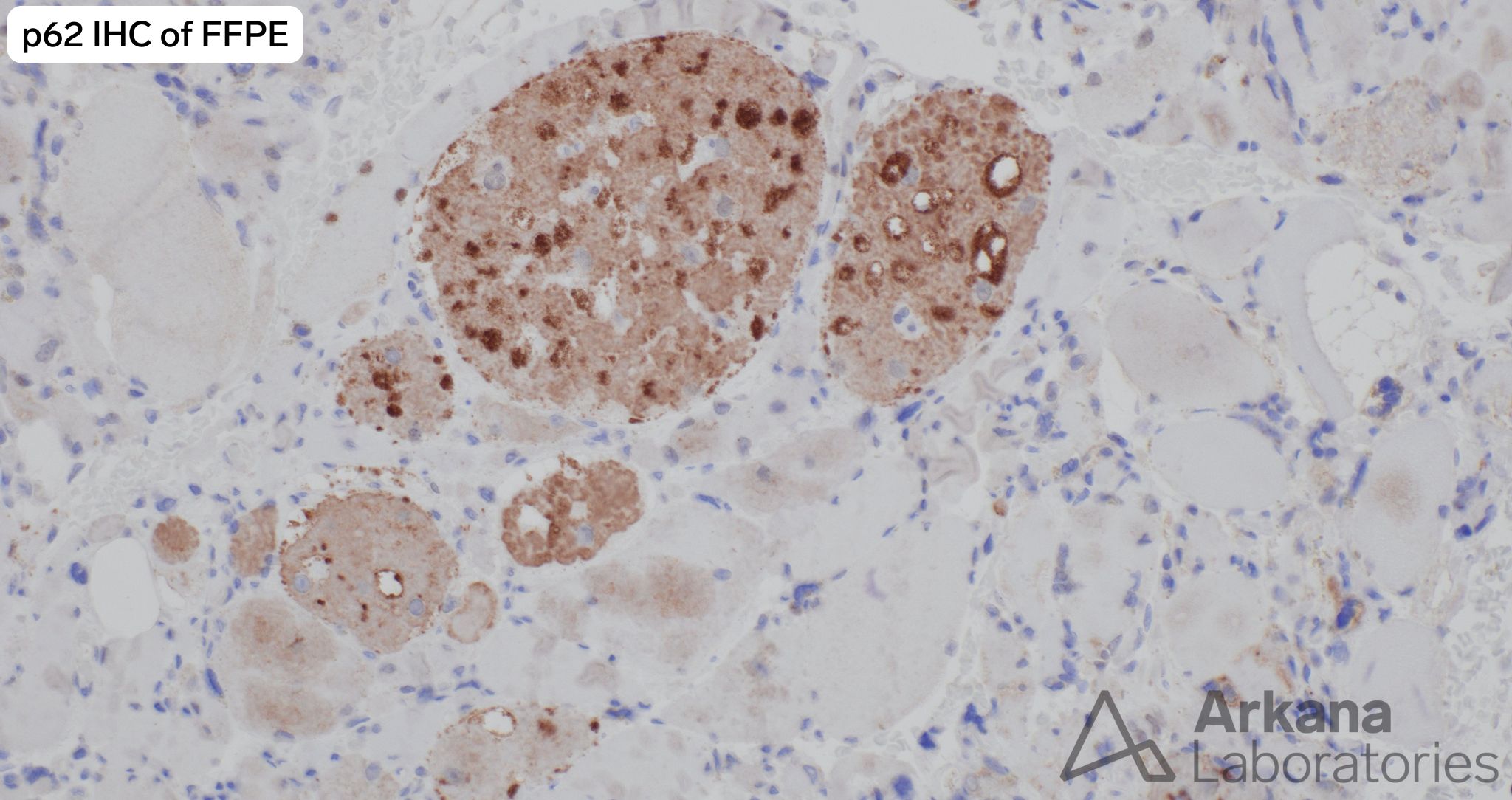
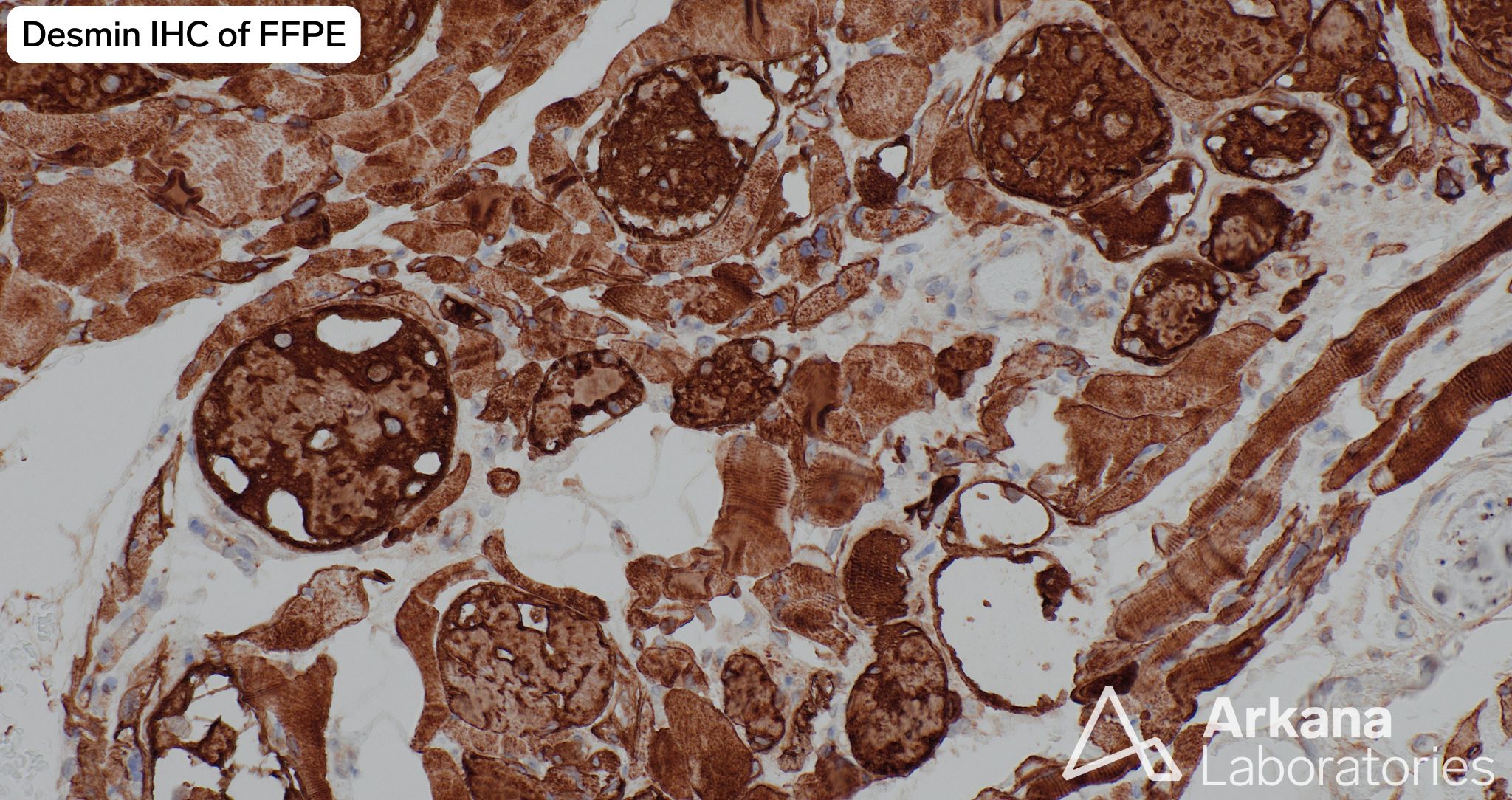
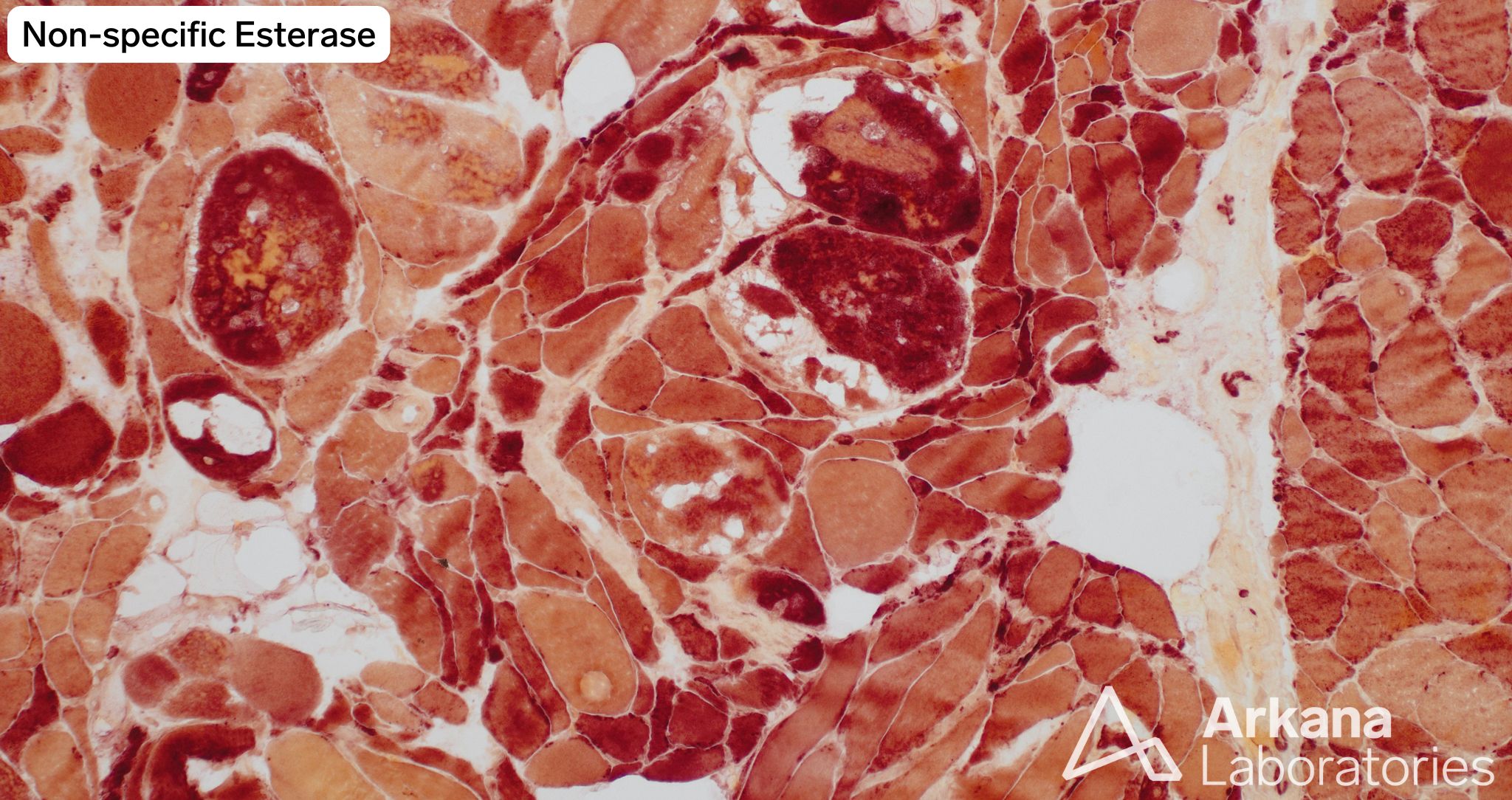
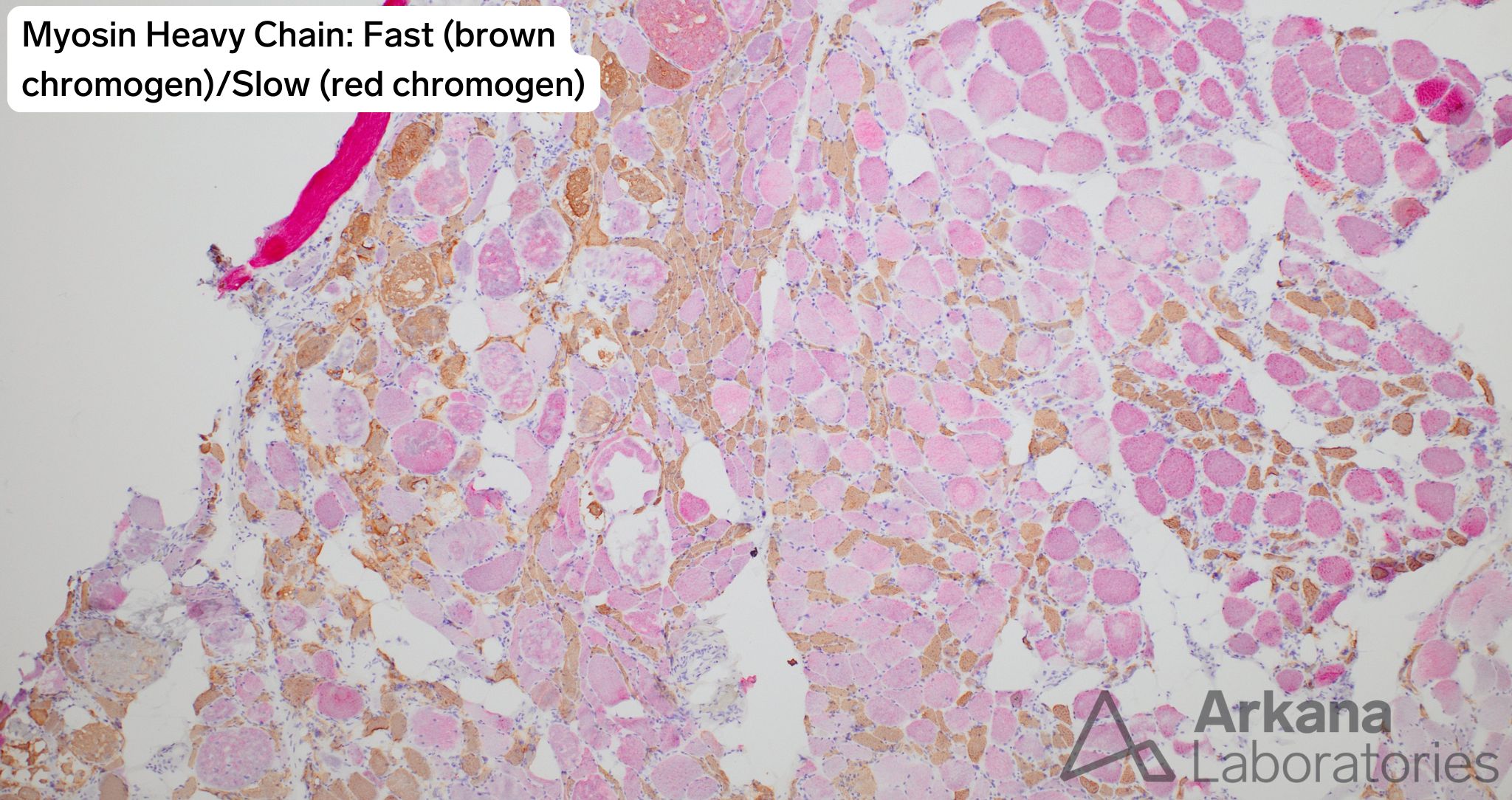
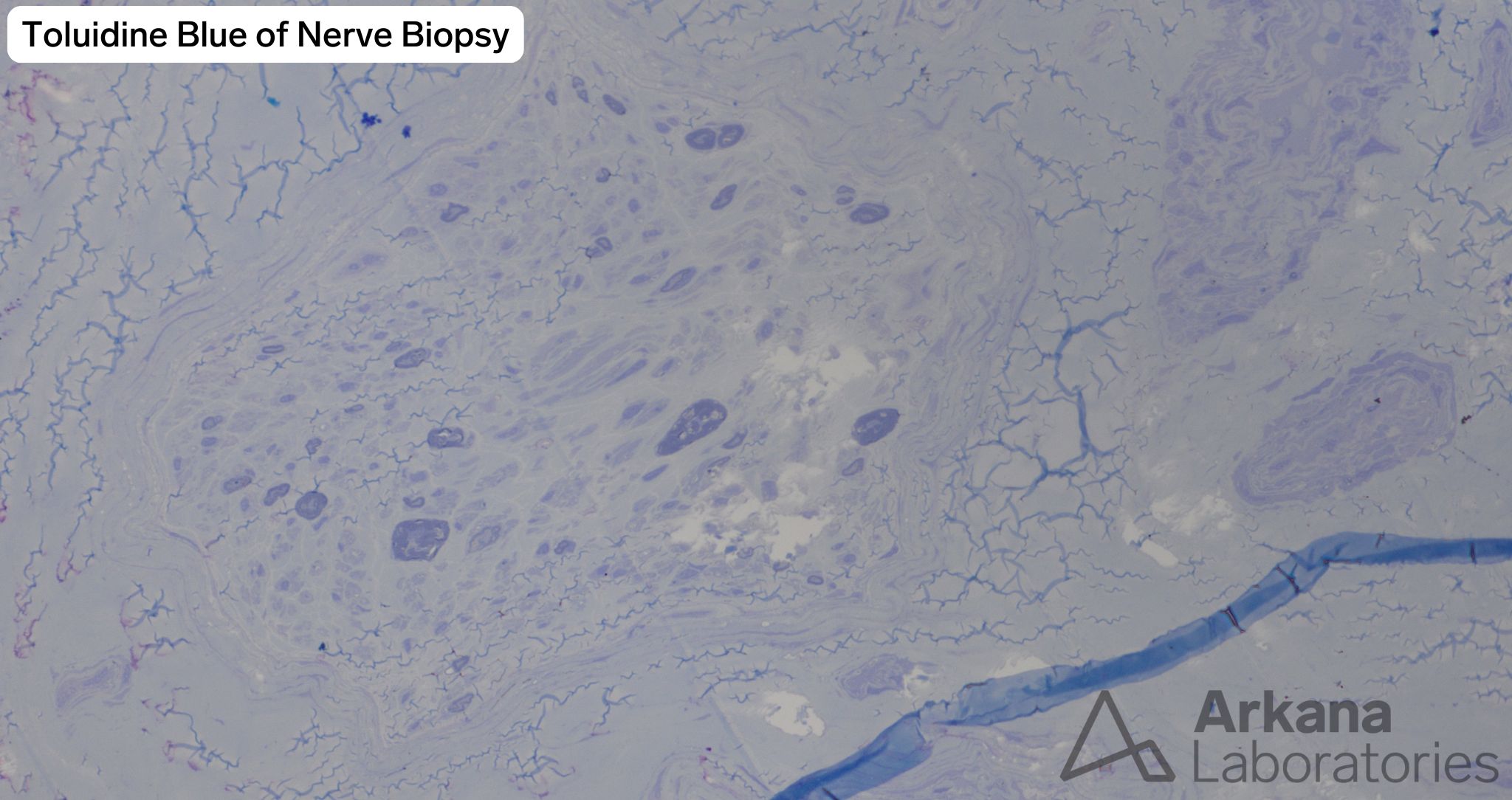
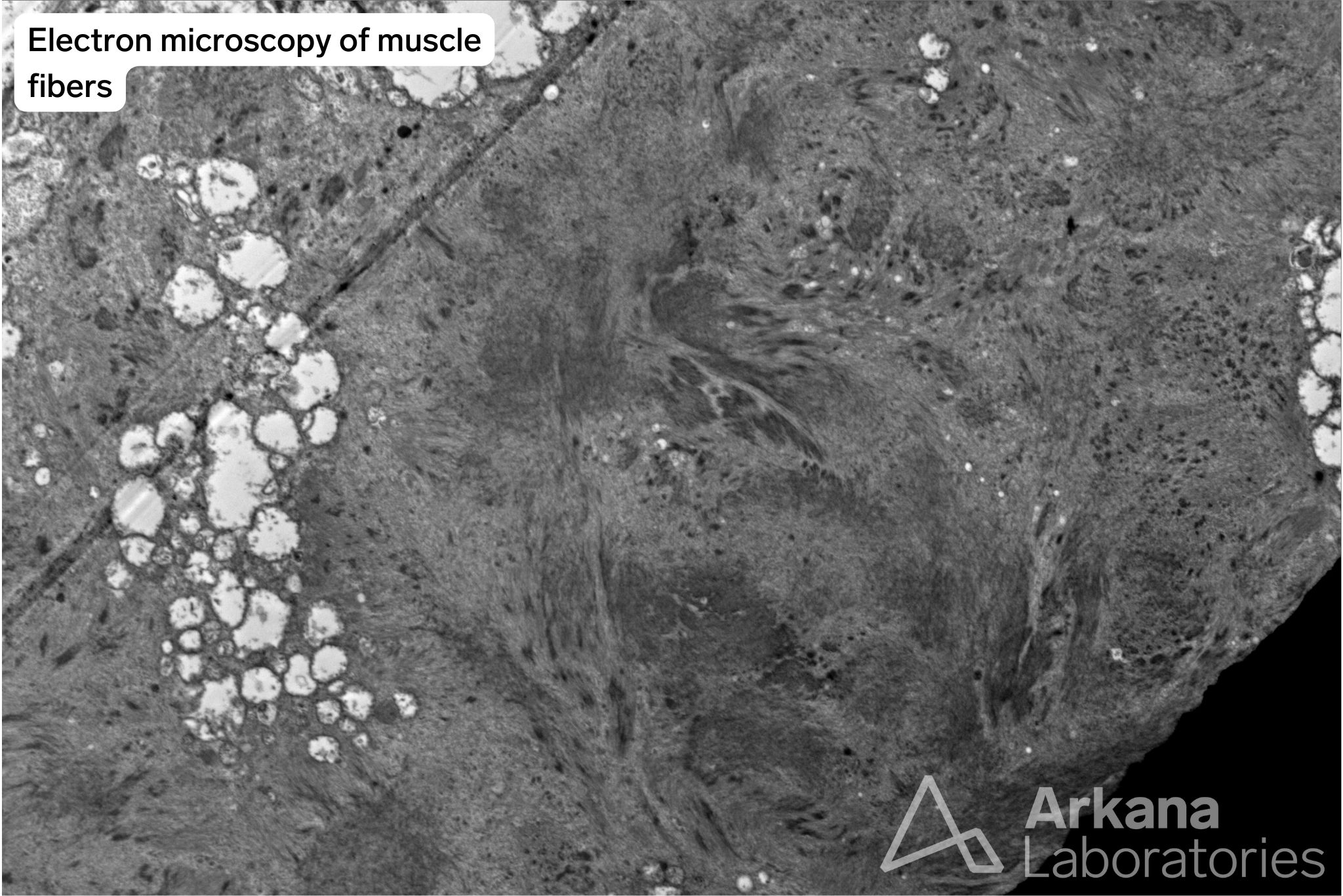
While signs of grouped atrophy, fiber type grouping, and small angulated fibers are present in the muscle fiber to support acute denervation and chronic reinnervation, there are extensive hypertrophied fibers demonstrating extensive sarcomeric disorganization and variable sarcoplasmic vacuolization with rare foci of sarcomeres being centrally displaced. These fibers are seen in both the FFPE and frozen specimen arguing against artefact. While the vacuoles stain for p62 and TDP-43, no significant inflammation is seen to support sIBM and the patient is noted to not be taking any steroids that may mask inflammation. The hypertrophied, disorganized fibers are strongly positive for desmin and the vacuoles stain red with GT and demonstrate darkly staining areas. The vacuolated fibers also demonstrate congophillia by immunofluorescence with the Texas Red filter. NADH, COX/SDH, and esterase staining demonstrate several fibers with a “rubbed-out” appearance. Electron microscopy of the muscle demonstrates disorganization of the myofibrillar apparatus with Z-line streaming. Together the findings are most supportive of answer choice D, a combination of neurogenic atrophy and myofibrillar myopathy.
Myofibrillar myopathy (MFM) represents a group of genetic diseases defined by myofibrillar disorganization, dissolution, and aggregated proteins (frequently desmin) and the frequent presence of vacuolated myofibers and often myofibers with a “rubbed out” appearance. The clinical presentation is quite heterogenous in MFMs and patients can present at any stage of life. These disorders are associated with mutations in an expanding list of genes which encode proteins involved in Z disc structure or function including: DES, CRYAB, MYOT, LDB3, FLNC, BAG3, FHL1, TTN, PYROXDI, and KY [1].
Reference(s) / Additional Reading:
- Luo YB, Peng Y, Lu Y, Li Q, Duan H, Bi F, Yang H. Front Neurol. 2020 Sep 15;11:1014.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.