The patient is a 42 y/o Southern Indian male who presents with longstanding, subnephrotic proteinuria, mild edema, and renal insufficiency.
Pick the most likely diagnosis and further testing required for diagnosis.
A. Fibronectin glomerulopathy, immunohistochemical staining for fibronectin
B. Collagenofibrotic Glomerulopathy, electron microscopy of deposits
C. Fibrillary Glomerulopathy, electron microscopy of deposits and routine immunofluorescence panel
D. AL-type Renal Amyloidosis, Congo red stain, and IHC/IF for kappa and lambda
E. Light Chain Deposition Disease, IHC/IF for kappa and lambda and electron microscopy of deposits
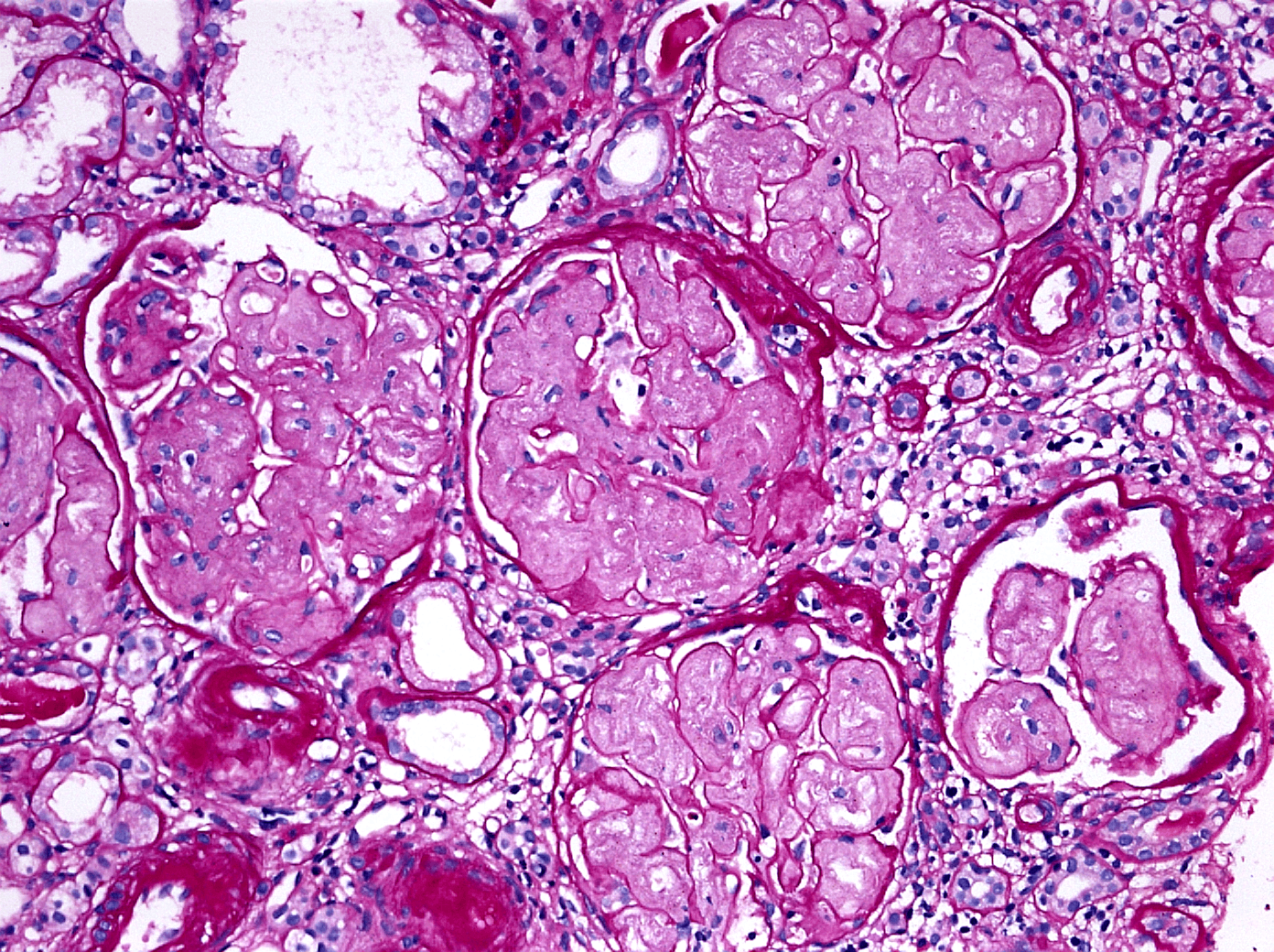
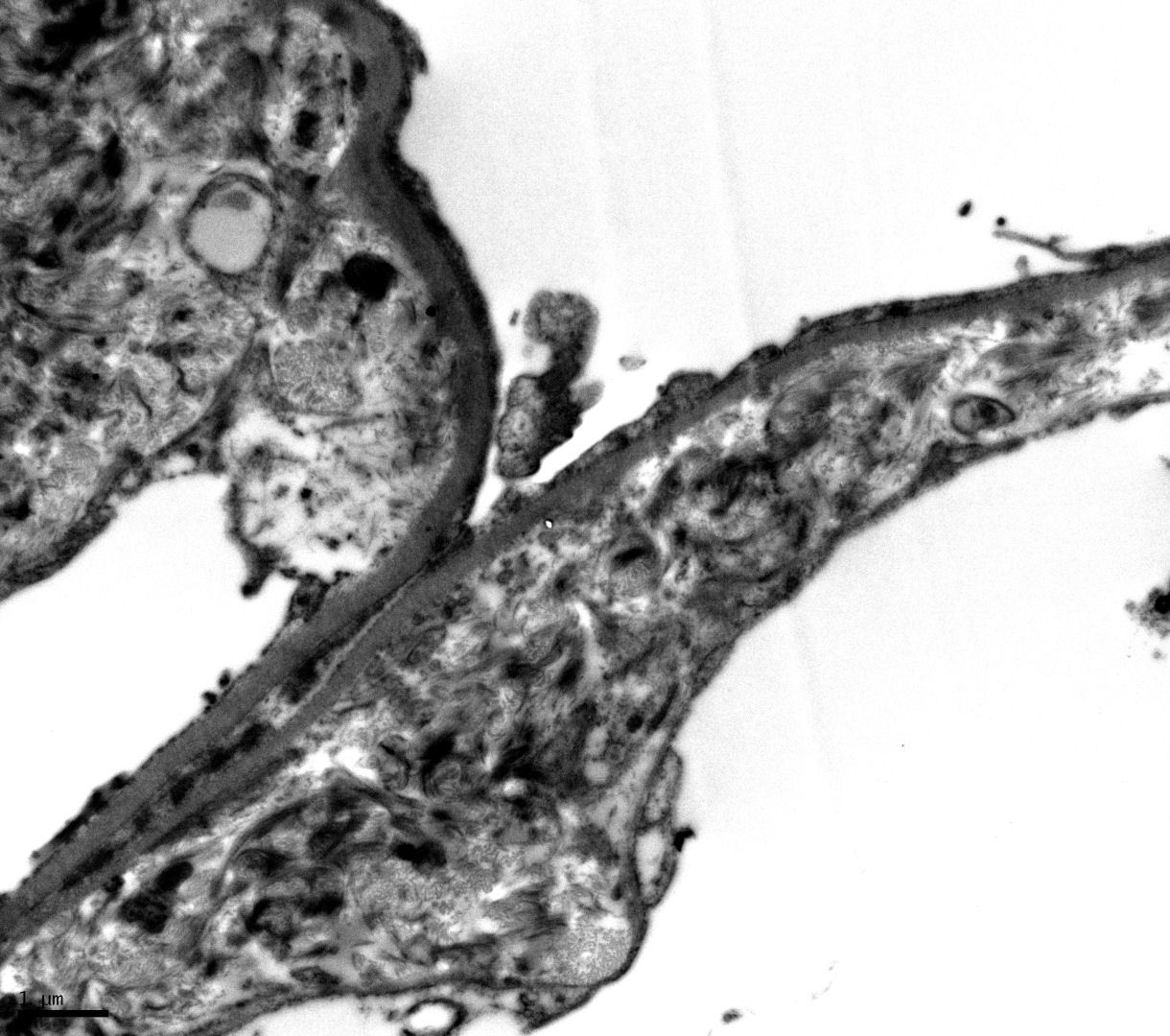
Answer: B. Collagenofibrotic glomerulopathy is a rare renal disease secondary to the deposition of type III collagen within the glomerulus and is of unknown etiology. This entity cannot be diagnosed by light microscopy alone and shares considerable morphologic overlap with fibronectin glomerulopathy. Electron microscopy showing stacked collagen bundles with fraying and curvilinear morphology confirms this diagnosis and IHC staining for type III collagen is helpful if available. Of note, most descriptions of the electron microscopy findings in collagenofibrotic glomerulopathy are described using tannic acid-lead or phosphotungstic acid preparation which shows the high detail, curvilinear fibrils within the mesangium and capillary walls that are most frequently seen in textbooks and the literature. However, as seen below, routine electron microscopy without these additives shows less detailed stacks of collagen with frayed edges and slight curvilinear morphology.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.