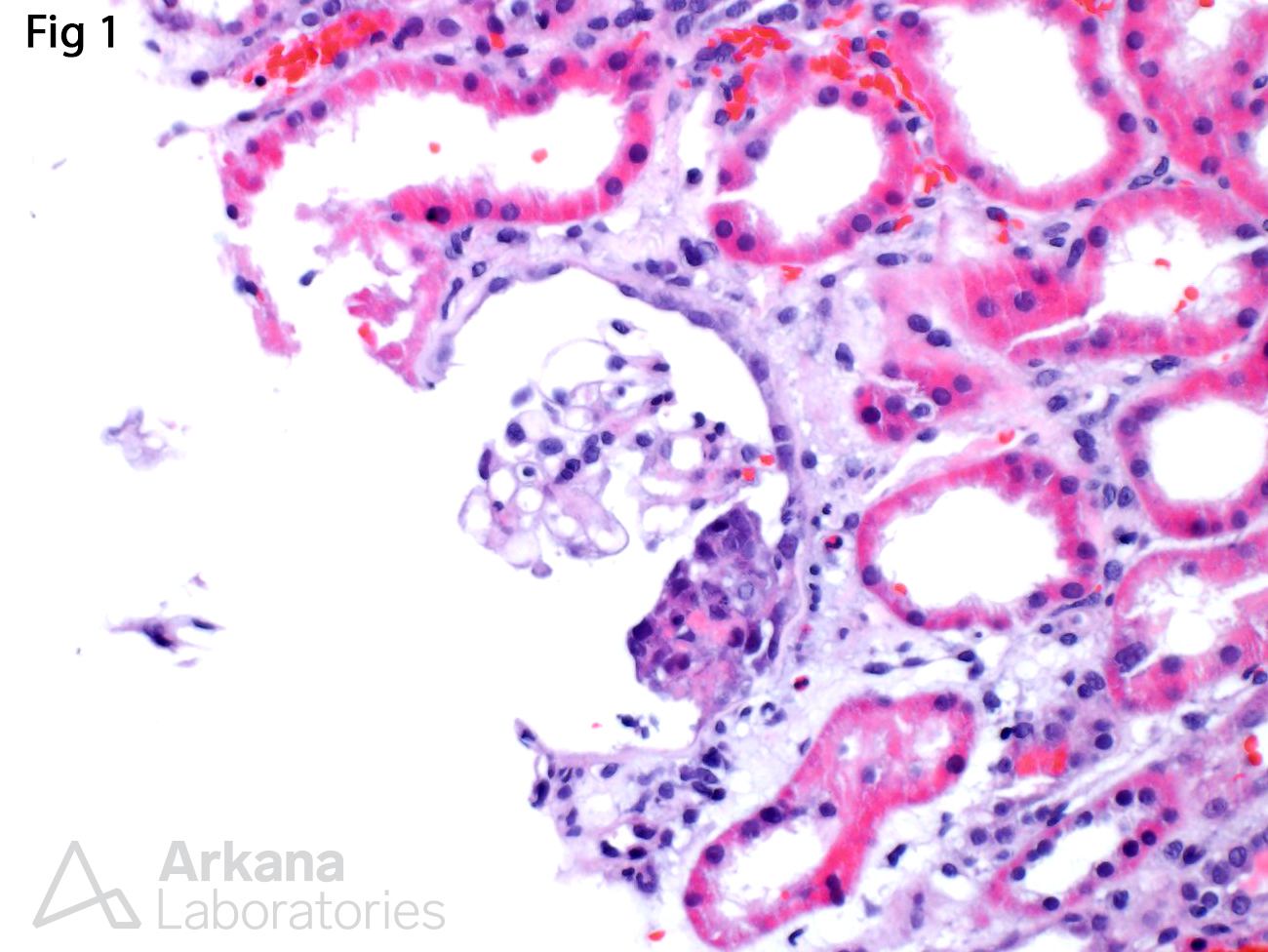
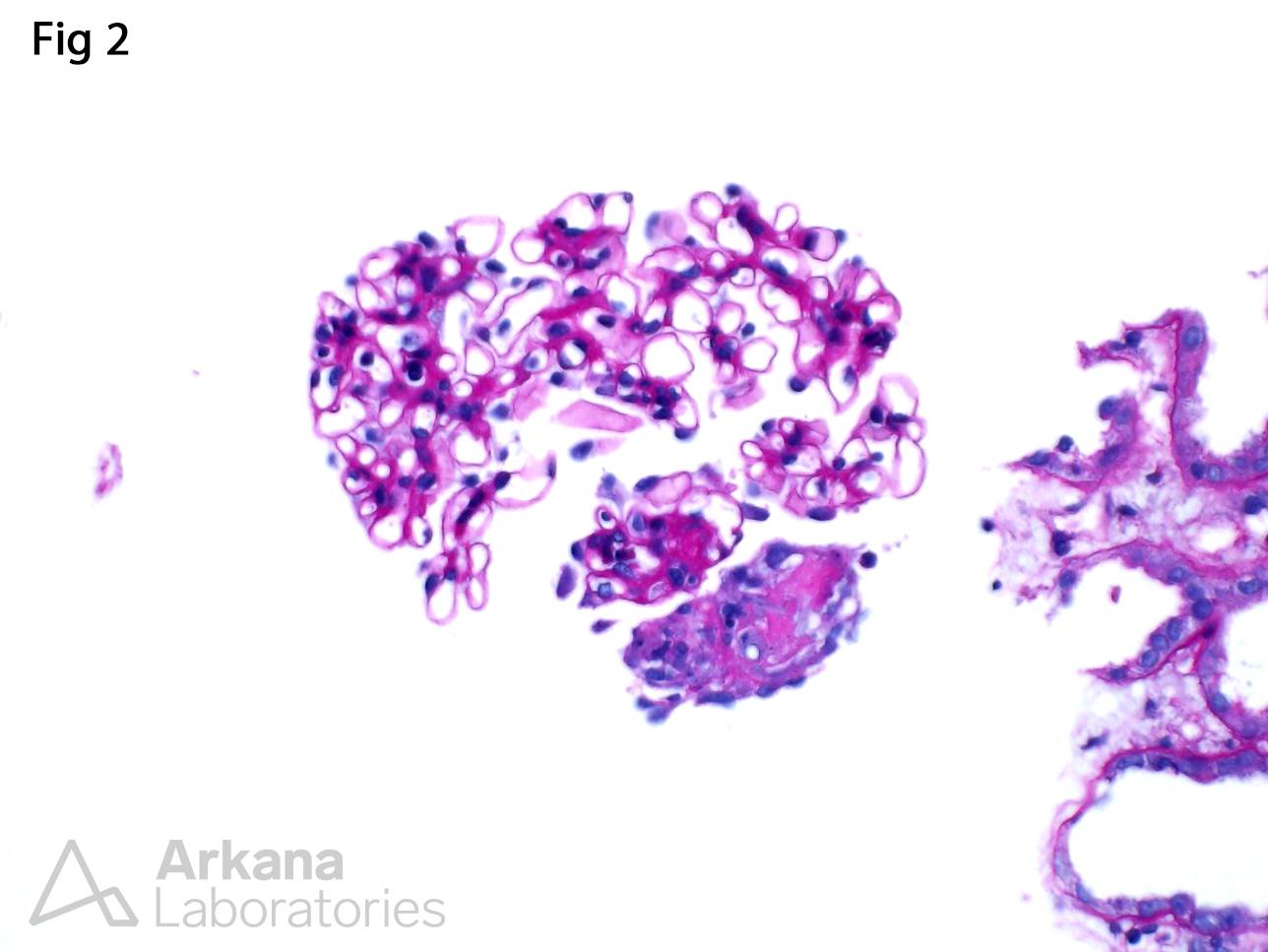
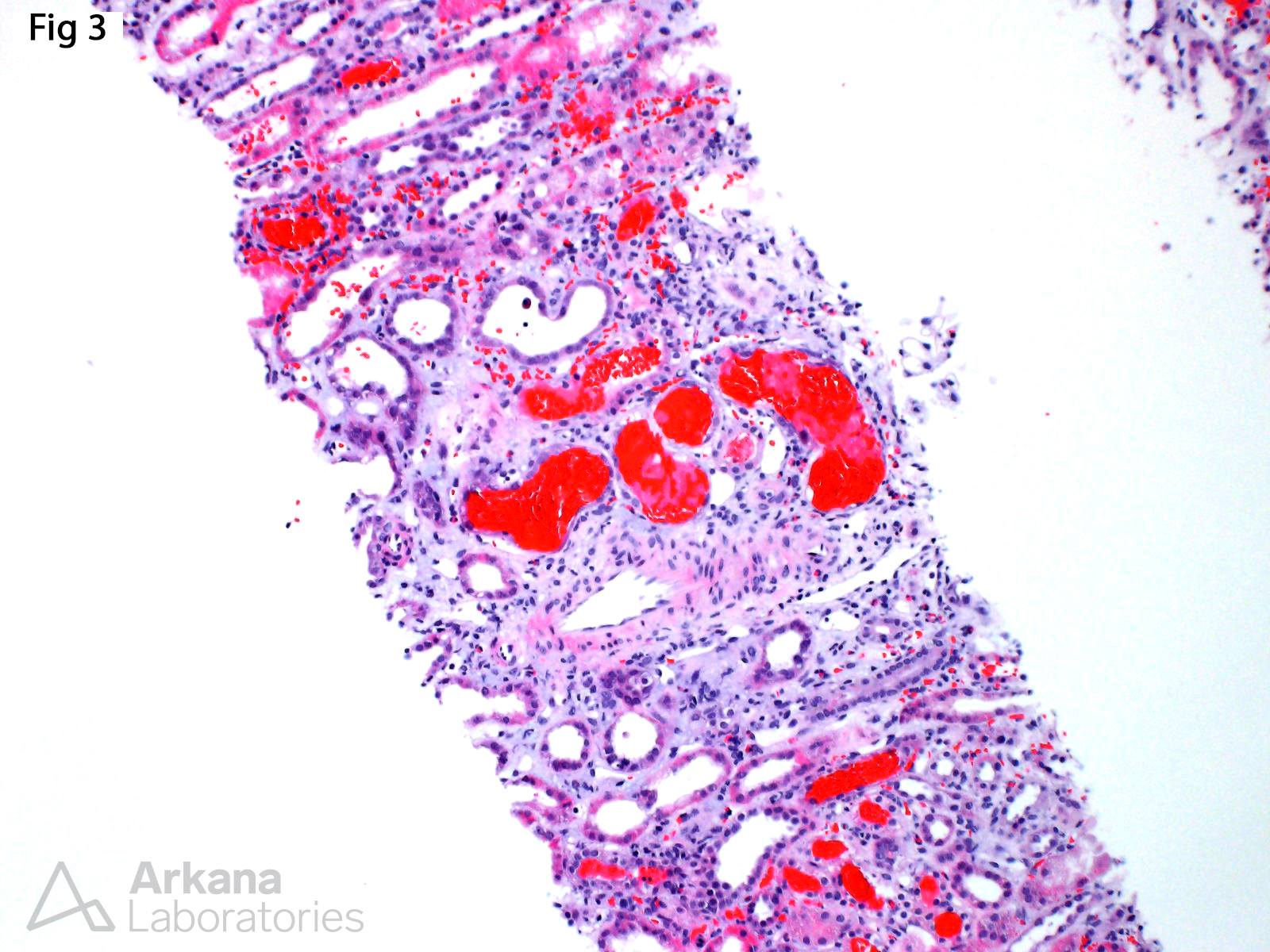
This renal biopsy was taken from a 35 year old male with history of intravenous drug abuse and MRSA tricuspid valve endocarditis, who developed acute kidney injury (Cr 4.7 mg/dl) and hematuria. The biopsy shows focal and segmental necrotizing and crescentic lesions involving approximately 10% of the available glomeruli (Fig 1 and 2). Additionally, there is severe acute tubular injury with numerous red blood cell casts (Fig 3). Immunofluorescence (not shown) reveals weak immune complex deposition within the spectrum of pauci-immune disease (IgA= 1+; IgM= trace; C3= 1+; Kappa= trace; lambda= 1+), and no definitive deposits were evident by electron microscopy. ANCA-mediated disease is the most common pathogenic mechanisms in cases of pauci-immune, focal necrotizing and crescentic glomerulonephritis; however, within the context of this patient’s clinical history, the biopsy findings are strongly favored to represent an endocarditis-associated glomerulonephritis. A large clinicopathologic series of cases of infective endocarditis-associated glomerulonephritis showed that the most common pattern of glomerular injury (seen in up to 53% of cases) is in the form of necrotizing and crescentic glomerulonephritis (See reference). Furthermore, 44% of the cases met criteria for pauci-immune disease. These results highlight the importance of including infective endocarditis-associated glomerulonephritis in the differential diagnosis of a pauci-immune necrotizing and crescentic glomerulonephritis and a transesophageal echocardiogram and infectious diseases consult may be warranted in patients at risk for infective endocarditis before implementation of aggressive immunosuppressive therapy.
Reference:
Boils CL, Nasr SH, Walker PD, et al. Update on endocarditis-associated glomerulonephritis. Kidney Int 2015; 87: 1241-1249.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.