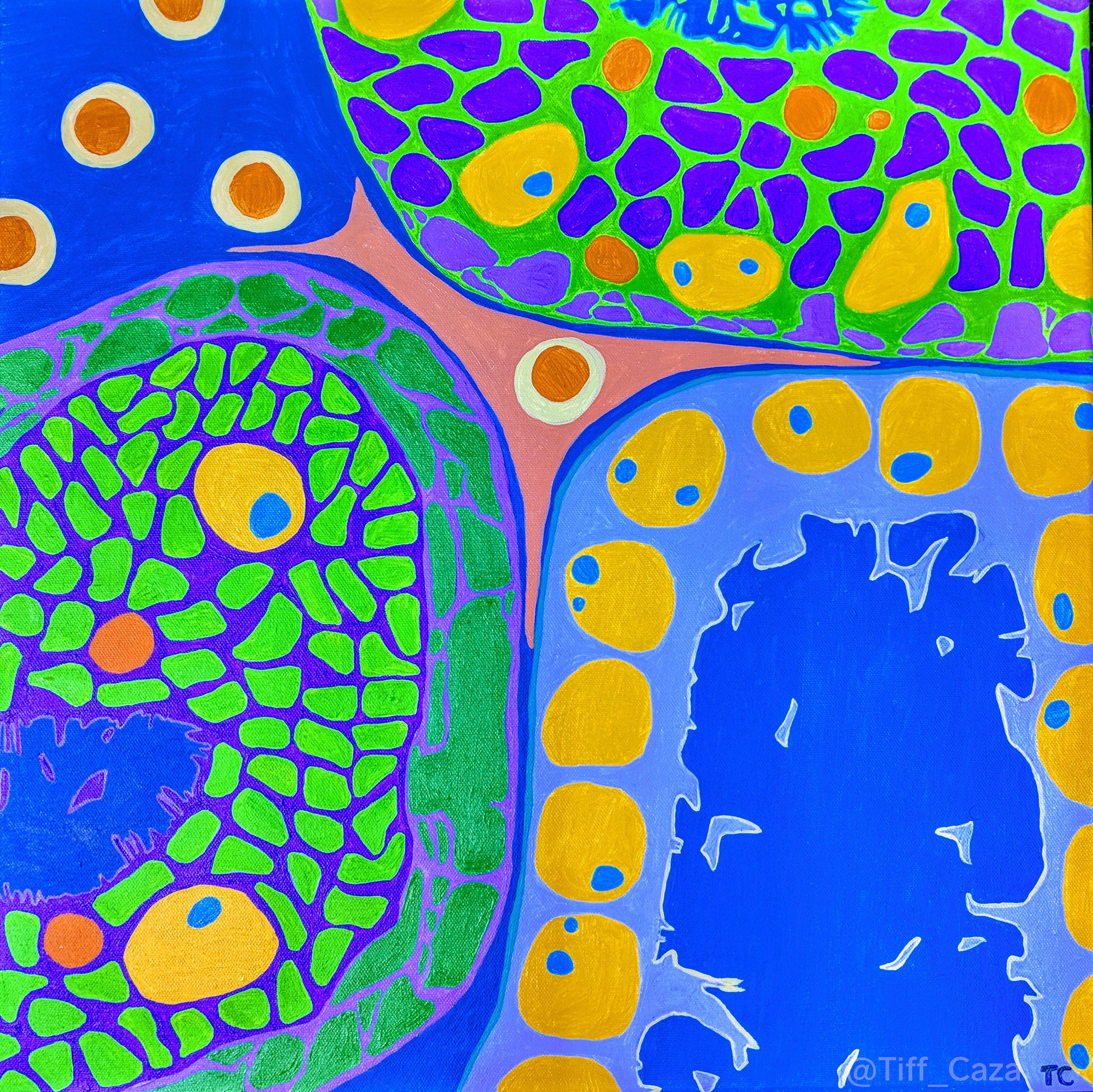
The above painting shows massive tubular basement membrane (electron dense on EM) deposits along proximal tubules with sparing of the distal tubules. This is a finding that can be seen by electron microscopy in anti-brush border antibody disease (ABBA). Tubular basement membrane deposits are also seen in lupus nephritis (all classes), IgG4-associated kidney disease, idiopathic hypocomplementemic interstitial nephritis, polyomavirus nephritis (BK virus or JC virus), or in response to certain medications (eculizumab, NSAIDS, and others). Interstitial inflammation is not prominent in ABBA disease, as it is with other pathologies with tubular basement membrane deposits (such as IgG4-associated disease, drug reactions, and polyomavirus nephritis).
Anti-brush border antibody disease is a rare cause of acute kidney injury or chronic renal failure in elderly individuals. It is caused by autoantibodies directed to the LDL receptor-related protein 2 (LRP2), also known as megalin (Larsen et al, 2018). An immunofluorescence stain for LRP2, highlighting tubular basement membrane deposits and proximal tubular brush border staining is shown below. All proximal tubules express LRP2 at their brush borders, but tubular basement membrane deposits are not normally present, and are seen in patients with ABBA. In addition to proximal tubular basement membrane deposits, ABBA patients also show segmental granular capillary loop staining along the glomerular basement membranes, corresponding to subepithelial deposits. Due to this segmental membranous glomerulopathy, ABBA patients often have proteinuria.
Anti-LRP2 antibodies circulate and can be detected in patient sera. Since the disease is caused by autoantibodies, immunosuppressive therapy may be helpful to delay the progression of chronic renal failure in ABBA patients.
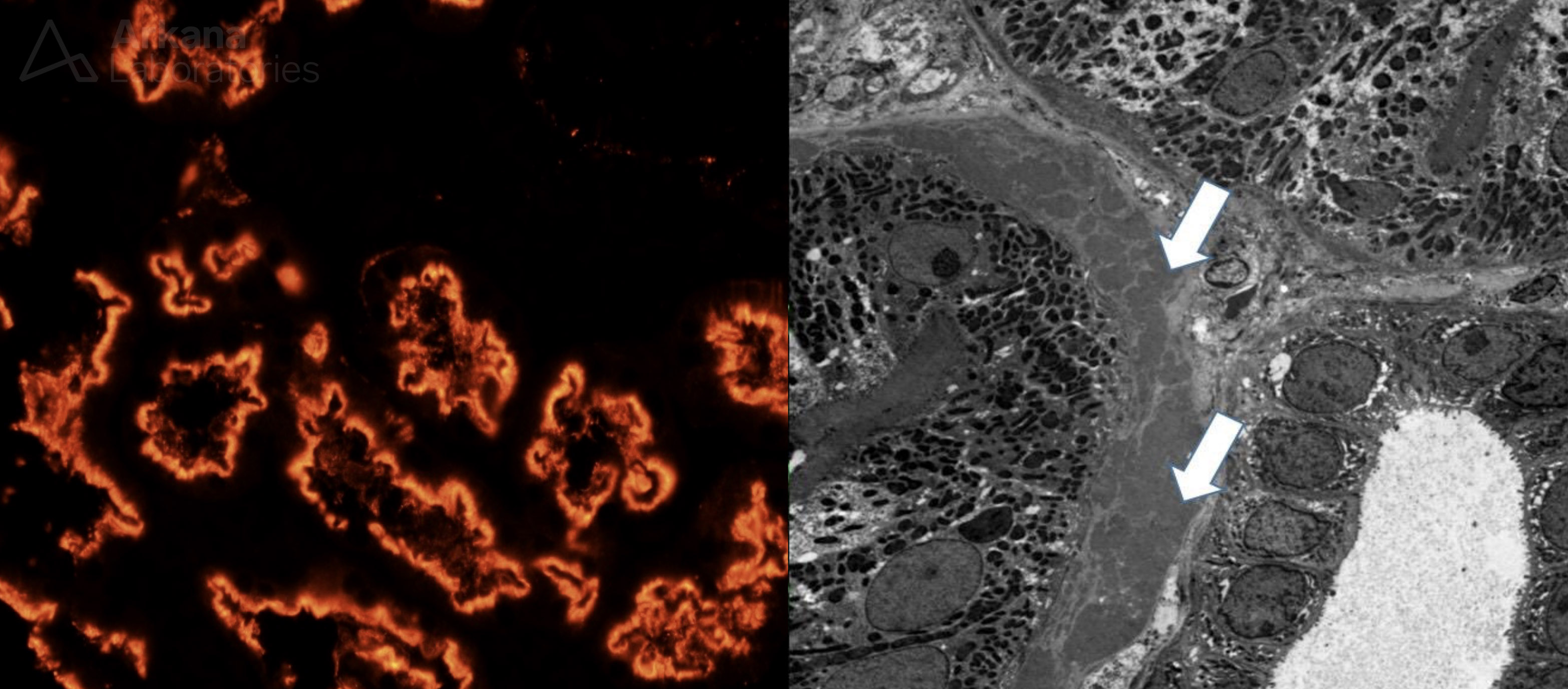
Histopathology of anti-brush border antibody disease. Left, Immunofluorescence for LRP2 (megalin), showing prominent brush border staining and small proximal tubular basement membrane deposits. Right, electron microscopy showing massive proximal tubular basement membrane deposits. Note the nearby distal tubule is without electron dense deposits.
Reference:
Larsen CP, Trivin-Avillach C, Coles P, Collins AB, Merchant M, Ma H, Wilkey DW, Ambruzs JM, Messias NC, Cossey LN, Rosales IA, Wooldridge T, Walker PD, Colvin RB, Klein J, Salant DJ, Beck LH. LDL receptor-related protein 2 (megalin) as a target antigen in human kidney anti-brush border antibody disease. J Am Soc Nephrol 2018 Feb; 29 (2): 644-653.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.

