
The above painting shows a glomerulus with capillary tuft collapse, visceral epithelial cell hyperplasia, and numerous protein resorption droplets within Bowman’s space; findings that can be seen in collapsing glomerulopathy. A PAS stain from a case of collapsing glomerulopathy is also shown in the photomicrograph below. Initially, collapsing glomerulopathy was considered a severe form of focal segmental glomerulosclerosis and placed into the Columbia classification. According to the Columbia classification, collapse of at least one capillary loop with obliteration of the lumen and proliferation and hypertrophy of overlying podocytes is sufficient for a diagnosis of the collapsing glomerulopathy. Tubulointerstitial damage is often concurrent but is not required for a diagnosis (D’Agati et al, 2004).
Patients with collapsing glomerulopathy present with rapidly progressive renal failure and nephrotic syndrome, with a higher rate of progression to end stage renal disease (ESRD) than traditional morphologies of focal and segmental glomerulosclerosis, with 47% of patients developing ESRD at 3 years (Farris et al, 2019). It is often resistant to corticosteroid therapy. If an underlying etiology is identified, treatment of the underlying condition can lead to disease remission in some patients.
Genetics can predispose to collapsing glomerulopathy in susceptible patients. Patients that are homozygous or compound heterozygous for APOL1 G1 and/or G2 risk alleles are most at risk. African Americans carry a higher frequency of G1 and G2 APOL1 alleles due to conferring resistance against trypanosomes that cause African sleeping sickness, and thus have an increased risk of collapsing glomerulopathy (as well as other APOL1-associated nephropathies). In addition to APOL1, other genetic risk factors for collapsing FSGS include CoQ10 deficiency (COQ2, COQ6), myoclonic epilepsy syndrome (SCARB2), Schimke immunoosseous dysplasia (SMARCAL1), mandibuloacral dysplasia (ZMPSTE24), Galloway-Mowat syndrome (WDR73), CD2AP deficiency, Charcot-Marie-Tooth disease (INF2), and TRPC6 mutations (an infantile form).
Collapsing glomerulopathy has also been associated with numerous other pathologies and potential etiologies and may require an initial ‘hit’ to develop kidney disease in some patients. These include vascular ischemia, drugs, infections, autoimmune diseases, and malignancies. A high frequency of collapsing glomerulopathy has been reported in the setting of thrombotic microangiopathies (Buob et al, 2016). Drugs associated with collapsing glomerulopathy include pamidronate, interferons, calcineurin inhibitors, anabolic steroids, griseofulvin, and heroin. Infections that can trigger collapsing glomerulopathy include HIV, HCV, CMV, HTLV-1, parvovirus B19, tuberculosis, malaria (Plasmodium falciparum), schistosomiasis, and filariasis (Loa Loa infection) (Cossey et al, 2017). Autoimmune diseases associated with collapsing glomerulopathy include systemic lupus erythematosus, Still disease, Behçet syndrome, and C1q nephropathy. Malignancies associated with collapsing glomerulopathy include leukemias, lymphomas, and multiple myeloma. Hemophagocytic lymphohistiocytosis, while not a hematologic malignancy, has also been associated with collapsing glomerulopathy.
One hypothesis for the etiology of segmental or total glomerular capillary tuft collapse is aberrant mitotic activity within podocytes resulting in a mitotic catastrophe. In this process, podocytes lose differentiation markers and enter the cell cycle (Shkreli et al, 2012). This has been reported in HIV-associated nephropathy, focal and segmental glomerulosclerosis, and with drug toxicity (particularly with Adriamycin use).
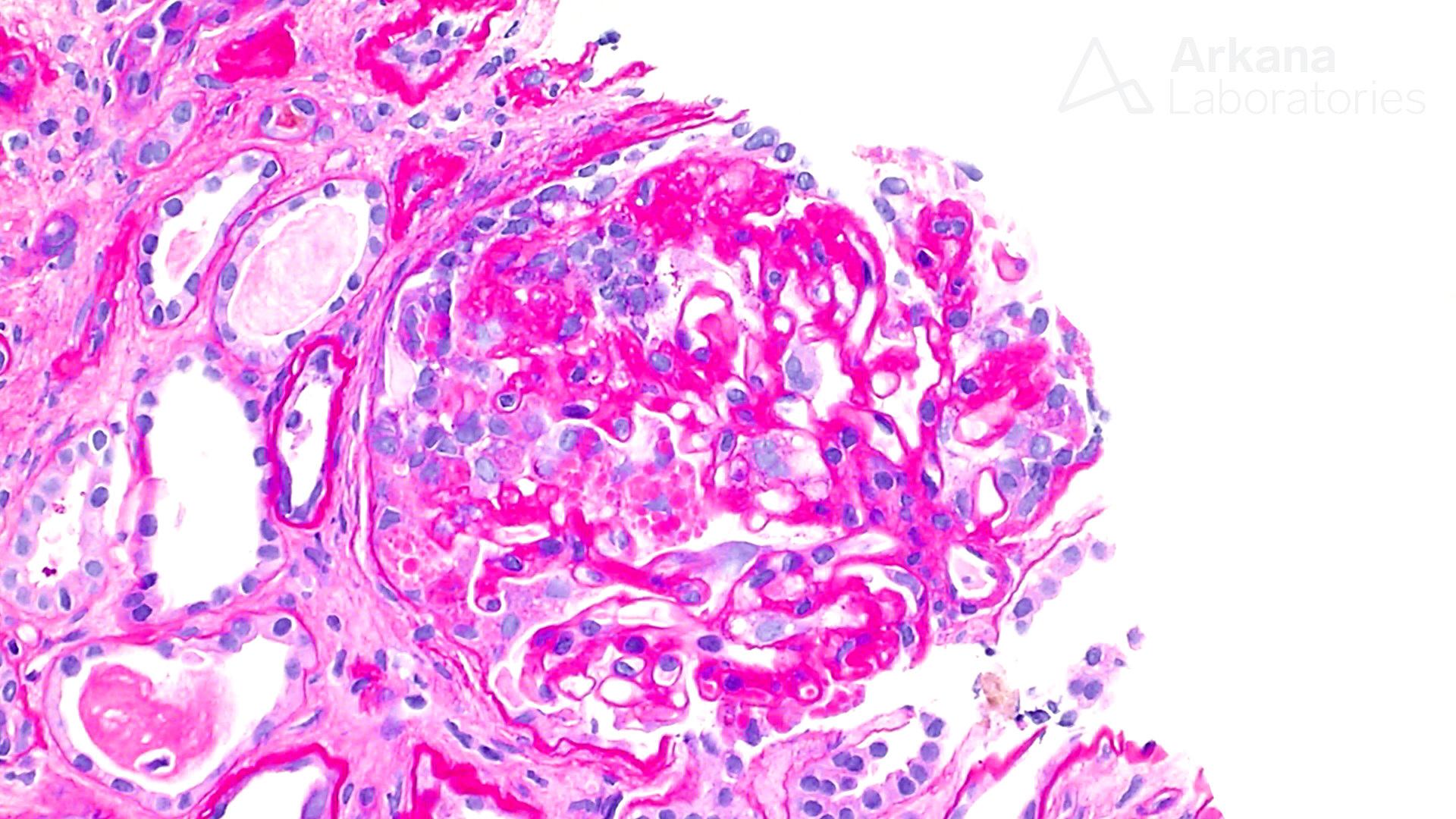
A PAS stain of a renal biopsy showing collapsing glomerulopathy.
References:
Buob D, Decambron M, Gnemmi V, Frimat M, Hoffman M, Azar R, Gheerbrant J-D, Guncestre T, Noel C, Copin M-C, Glowacki F. Collapsing glomerulopathy is common in the setting of thrombotic microangiopathy of the native kidney. Kidney International 2016 Dec; 90 (6): 1321-1331.
Cossey LN, Larsen CP, Liapis H. Collapsing glomerulopathy: a 30-year perspective and single, large center experience. Clinical Kidney Journal 2017 Aug; 10 (4): 443-449.
D’Agati VD, Fogo AB, Bruijn JA, Jennette JC. Pathologic classification of focal segmental glomerulosclerosis: a working proposal. Am J Kidney Dis. 2004 Feb;43(2):368-82.
Farris AB, Weins A. Collapsing Glomerulopathy. Diagnostic Pathology: Kidney Diseases 3rd Ed. 2019; Quebec, Canada: Elsevier; pp 70-79
Shkreli M, Sarin KY, Pech MF, Papeta N, Chang W, Brockman SA, Cheung P, Lee E, Kuhnert F, Olson JL, Kuo CJ, Gharavi AG, D’Agati VD, Artandi SE. Reversible cell-cycle entry in adult kidney podocytes through regulated control of telomerase and Wnt signaling. Nature Medicine 2012; 18: 111-119.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.

