Tuesday:
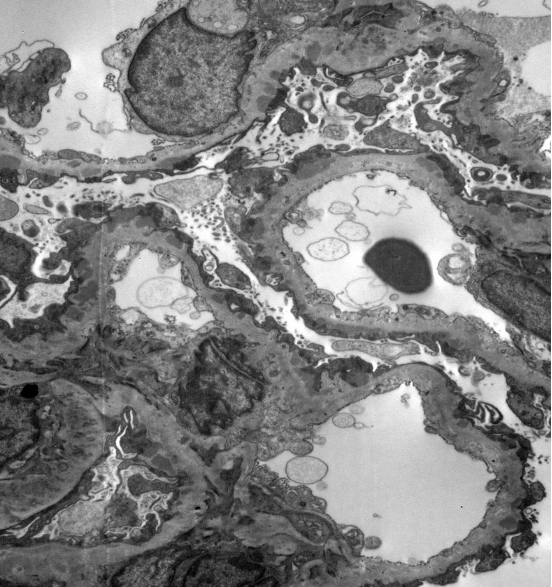
Let’s start with a poll. You have a 25-year-old female patient with a positive ANA and proteinuria. On a kidney biopsy, light microscopy looks fairly unremarkable – a little mesangial expansion and mildly prominent capillary loops. IF is also nearly unremarkable, but with 2+ C3 staining. On EM, you have this finding.
What do you do next?
- Stain the biopsy with PLA2R
- Perform IgG subclasses
- Do paraffin immunofluorescence
- There has to be a mix-up – check with the lab
Answer – Paraffin Immunofluorescence
What do you expect to find by paraffin immunofluorescence?
- Strong C3 staining to confirm C3 glomerulopathy
- IgG and kappa light chain staining
- IgG and lambda light chain staining
- Either B or C
Answer – IgG and kappa light chain staining
You perform immunostaining for serum amyloid P and find strong staining along the glomerular capillary loops, with some mesangial staining as well. What is your diagnosis?
- Membranous glomerulopathy, favor primary
- Membranous glomerulopathy, favor secondary
- Membranous glomerulopathy with masked IgG kappa deposits
- C3 glomerulopathy
Answer- Membranous glomerulopathy with masked IgG kappa deposits
Let’s learn more! It’s time for another disease week @arkanalabs. We’ll take a deep dive into the disease, membranous-like glomerulopathy with masked IgG kappa deposits throughout the week. Follow along with #DiseaseWeek
Membranous-like Glomerulopathy with Masked IgG kappa Deposits (MGMID) is an immune complex-mediated kidney disease, usually affecting young women.

We will be primarily discussing data from the following papers and share the highlights, but here are the links to learn more.
https://www.ncbi.nlm.nih.gov/pubmed/24429395
https://www.ncbi.nlm.nih.gov/pubmed/29142932
https://www.kidney-international.org/article/S0085-2538(19)31119-6/pdf
https://pubmed.ncbi.nlm.nih.gov/24978376/
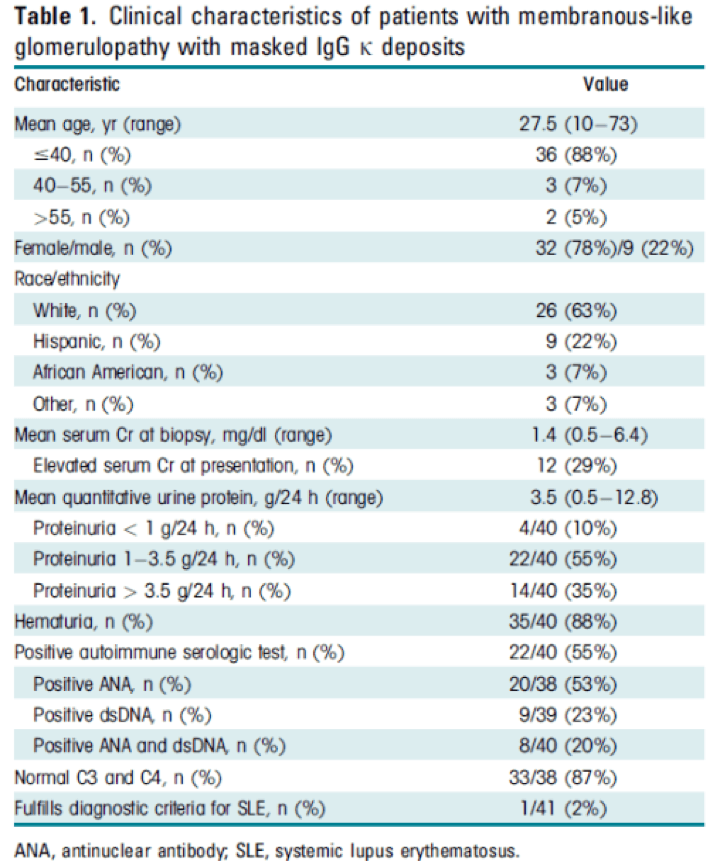
MGMID is very rare, making up only 0.1% of kidney biopsies (41/42,711 biopsies in a 5 year period).
Some patients with MGMID have a positive ANA or vague autoimmune manifestations, but most do not have a clinical diagnosis of SLE. They typically undergo kidney biopsy for proteinuria, which can be nephrotic range.
Wednesday:
Microscopic features of MGMID. On light microscopy, the glomerular capillary loops appear prominent and there are fuscinophilic deposits on trichrome stain (a) and may be the formation of spikes and holes on silver stains (b), as also seen in membranous glomerulopathy (it’s membranous-like).
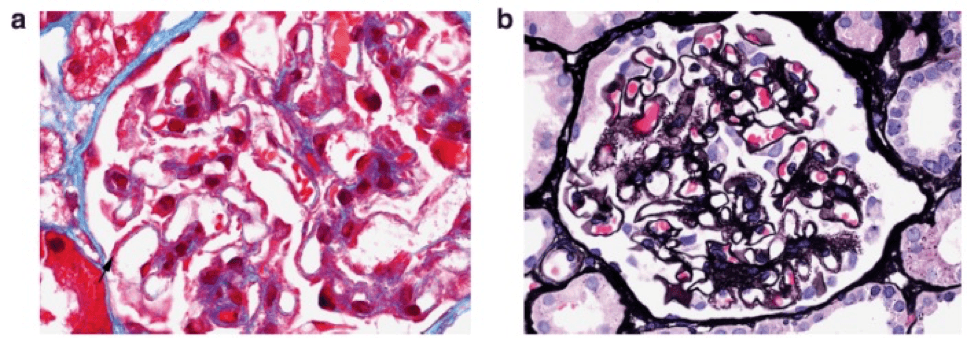
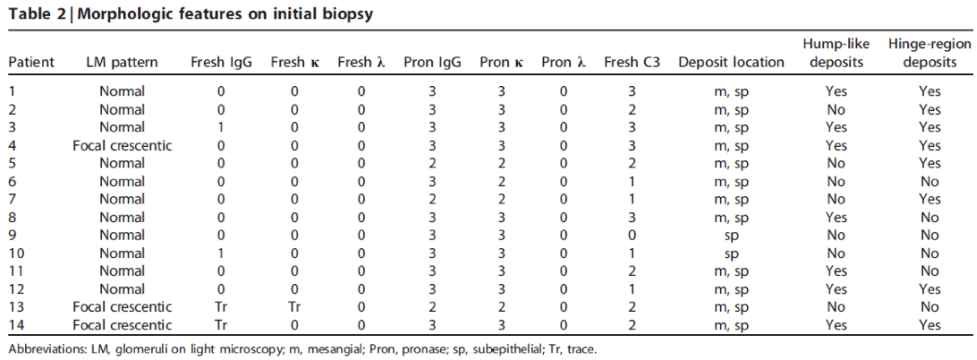
On immunofluorescence microscopy, IgG is negative in a majority of cases (a). However, pronase digestion on FFPE tissue will lead to “unmasking” of immune deposits, which will be positive along the glomerular capillary loops and frequently also within the mesangium (b).
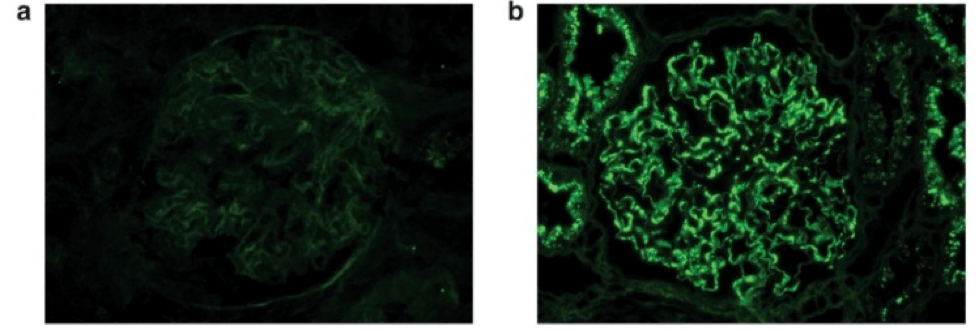
There is unmasked kappa (c), but not lambda (d), light chains in the same distribution as IgG on paraffin immunofluorescence.
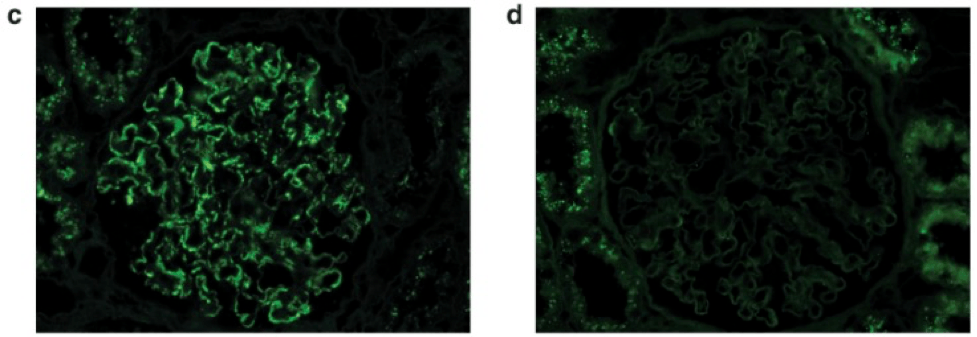
Immunofluorescence results from 41 cases of MGMID are shown in the table below.
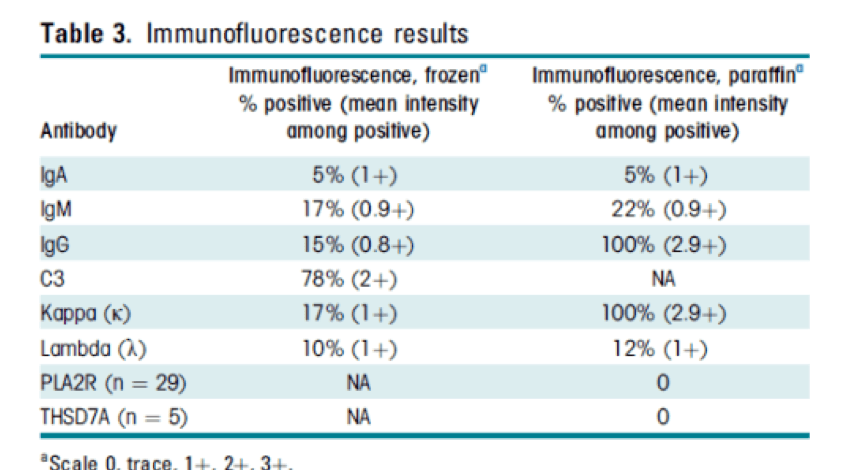
Electron microscopy often shows subepithelial and intramembranous deposits, and frequently also shows mesangial immune deposits.
C3 immunofluorescence staining is common on standard immunofluorescence in cases of MGMID.
You should consider a diagnosis of MGMID when there is only C3 staining on routine immunofluorescence, but a membranous-like pattern by electron microscopy. Performing paraffin IF will unmask immune deposits.
Some patients will not have masked IgG kappa and will have deposits seen on routine immunofluorescence. In these cases, IgG subclasses can be performed, and the deposits will be IgG1 restricted.
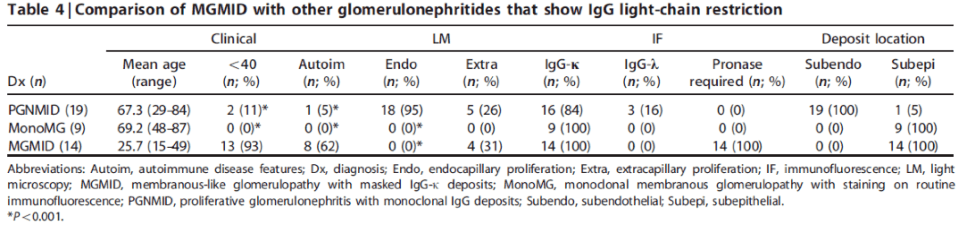
MGMID can be distinguished from PGMID by the lack of endocapillary proliferation and subendothelial deposits. Unlike monoclonal membranous glomerulopathy, MGMID typically has masked IgG deposits.
Thursday:
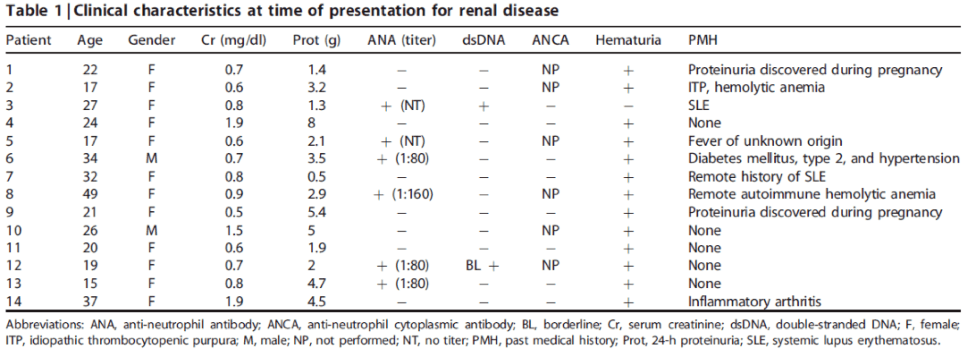
A larger cohort of 41 patients showed female predominance (78%) and a clinical presentation with proteinuria, microscopic hematuria, and often a positive ANA without clinical features of lupus.
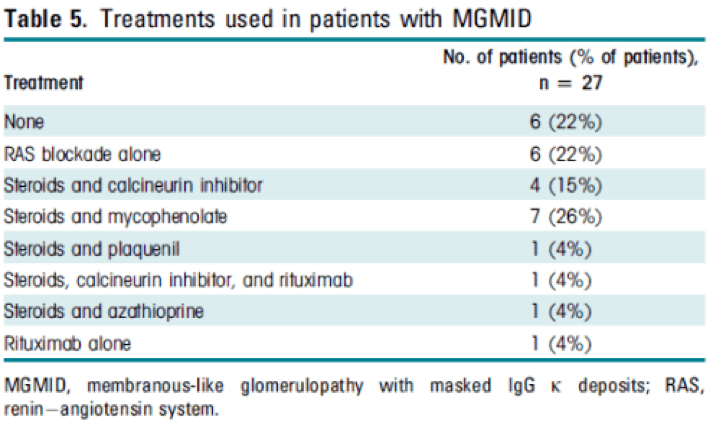
Treatment varied among patients and the optimal therapy for this disease is currently unknown.
Friday:
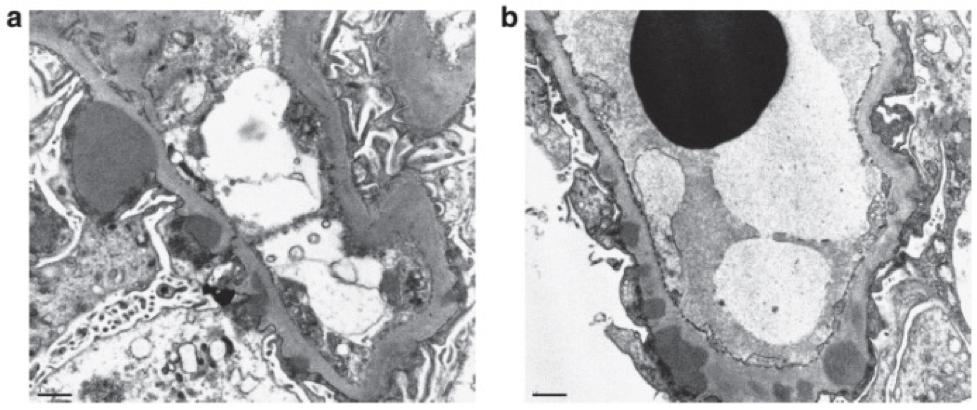
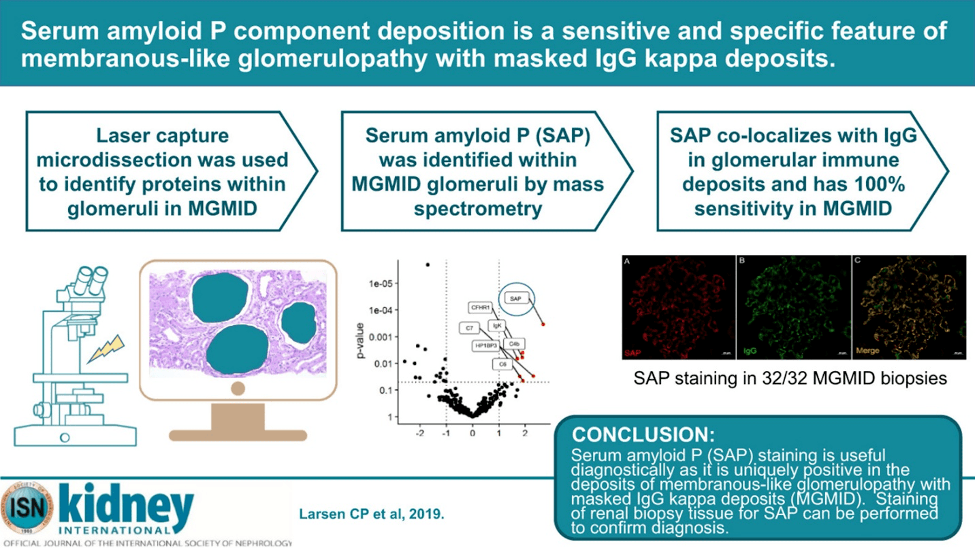
Laser capture microdissection followed by mass spectrometry identified serum amyloid P (SAP) as uniquely present within glomeruli in MGMID.
SAP was expressed in a granular capillary loop (and sometimes mesangial) pattern within glomeruli and showed co-localization with IgG within glomerular deposits (c). PLA2R positive membranous glomerulopathy is shown in the bottom panels as a negative control, which shows no staining within glomeruli.
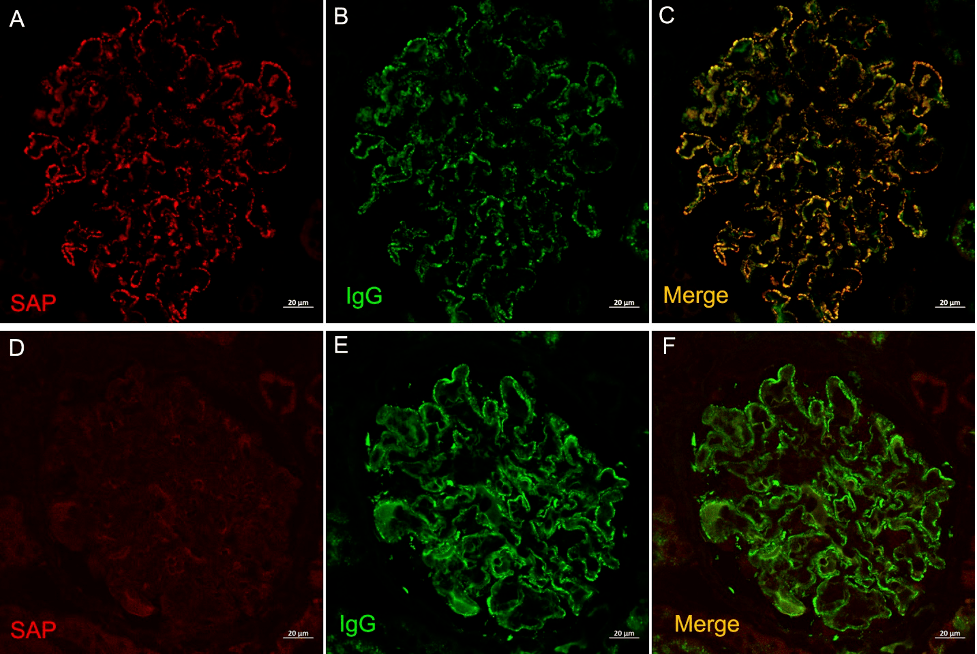
SAP staining of multiple glomerular diseases, including C3 glomerulonephritis, dense deposit disease, fibrillary glomerulonephritis, IgA nephropathy, PLA2R or THSD7A positive MG, infection-associated glomerulonephritis, cryoglobulinemic glomerulonephritis, membranous lupus nephritis, proliferative lupus nephritis, and PGMID were all negative but were positive in all (32/32) cases of MGMID, showing high specificity. #DiseaseWeek
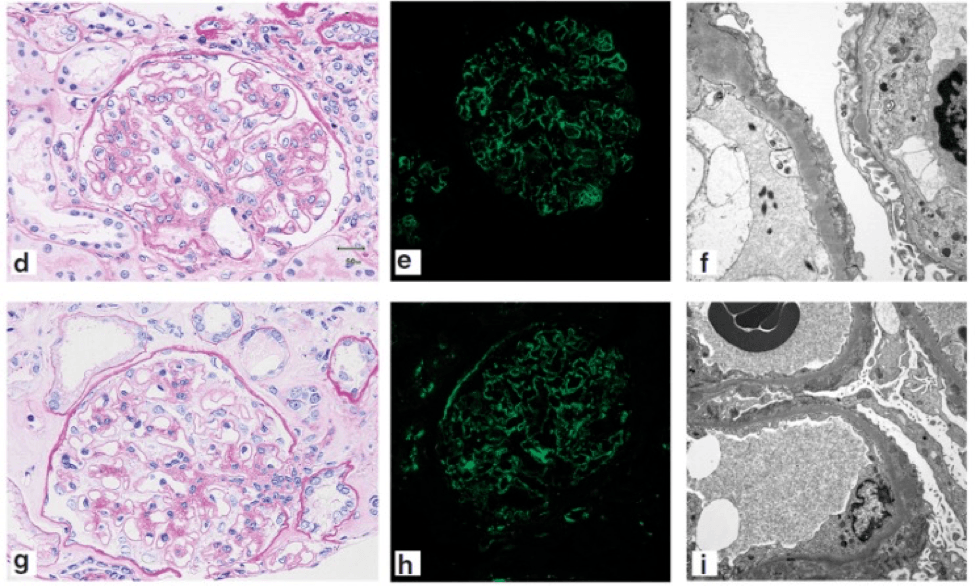
This is helpful to have this biomarker as morphologically, there are mimics of MGMID. Here’s C3 glomerulopathy (top) and PLA2R-positive MN (bottom), and you can notice identical light, standard IF, and EM findings that occur in MGMID. #DiseaseWeek
https://pubmed.ncbi.nlm.nih.gov/24978376/
The reason for the light chain restriction in MGMID is unknown, but this is not thought to be an MGRS lesion, rather an autoimmune disease.
There are no reported cases of MGMID being associated with a MGUS or underlying lymphoproliferative disorder/plasma cell dyscrasia. Instead, autoimmunity is directed against SAP, which of which IgG1 kappa is within its interactome.
SAP staining by paraffin immunofluorescence of kidney biopsies is a useful diagnostic tool for MGMID, which is both sensitive and specific.
Thank you for following along to our #DiseaseWeek on membranous-like glomerulopathy with masked IgG kappa deposits @Arkanalabs.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.