About Us
Arkana is a learning, teaching, innovating practice with one unifying passion: to work toward research breakthroughs that make our services unnecessary.
Learn About Our PracticePopular Posts

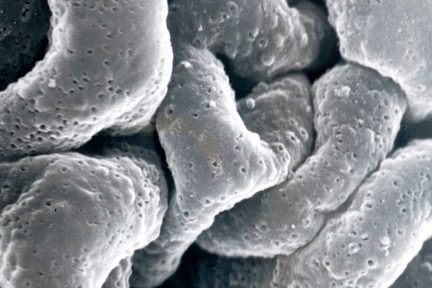
Kidneys for Kids
What are the kidneys and what do they do? Your kidneys are organs shaped like beans (think kidney beans) and…
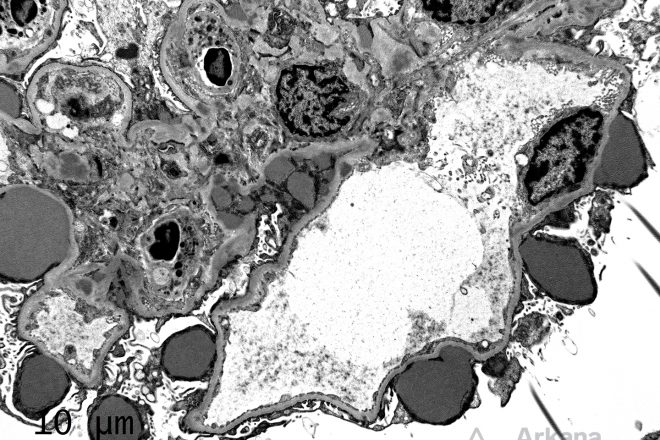
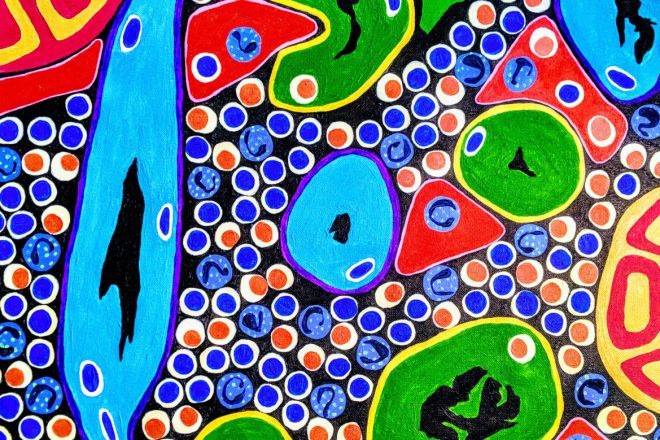
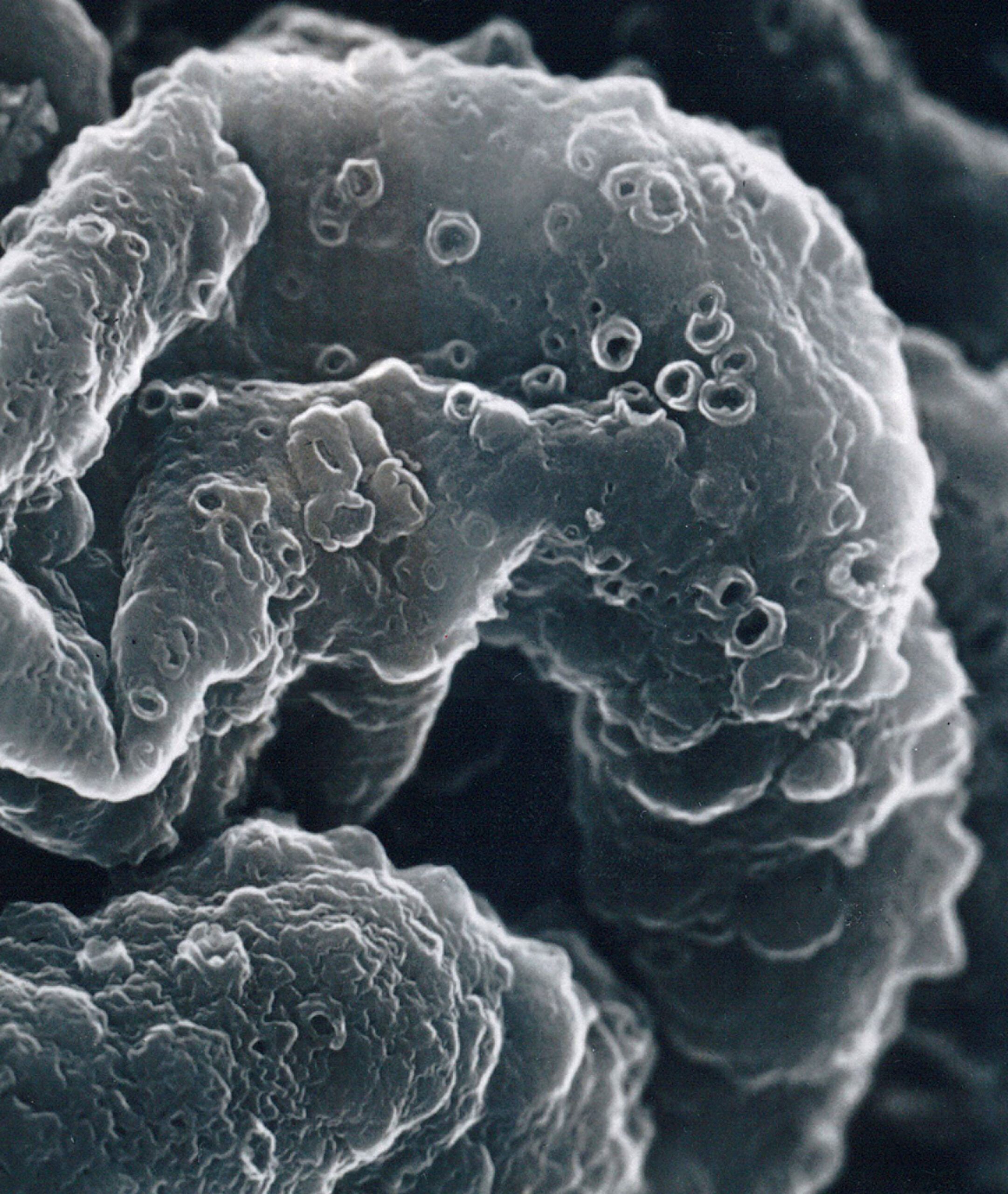
“Pinholes” on Silver Stain
Todays eyeSCANdy image shows acellular scanning EM from a biopsy with membranous glomerulonephritis, stage I with numerous small shallow depressions…
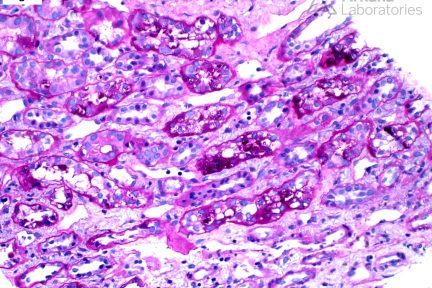
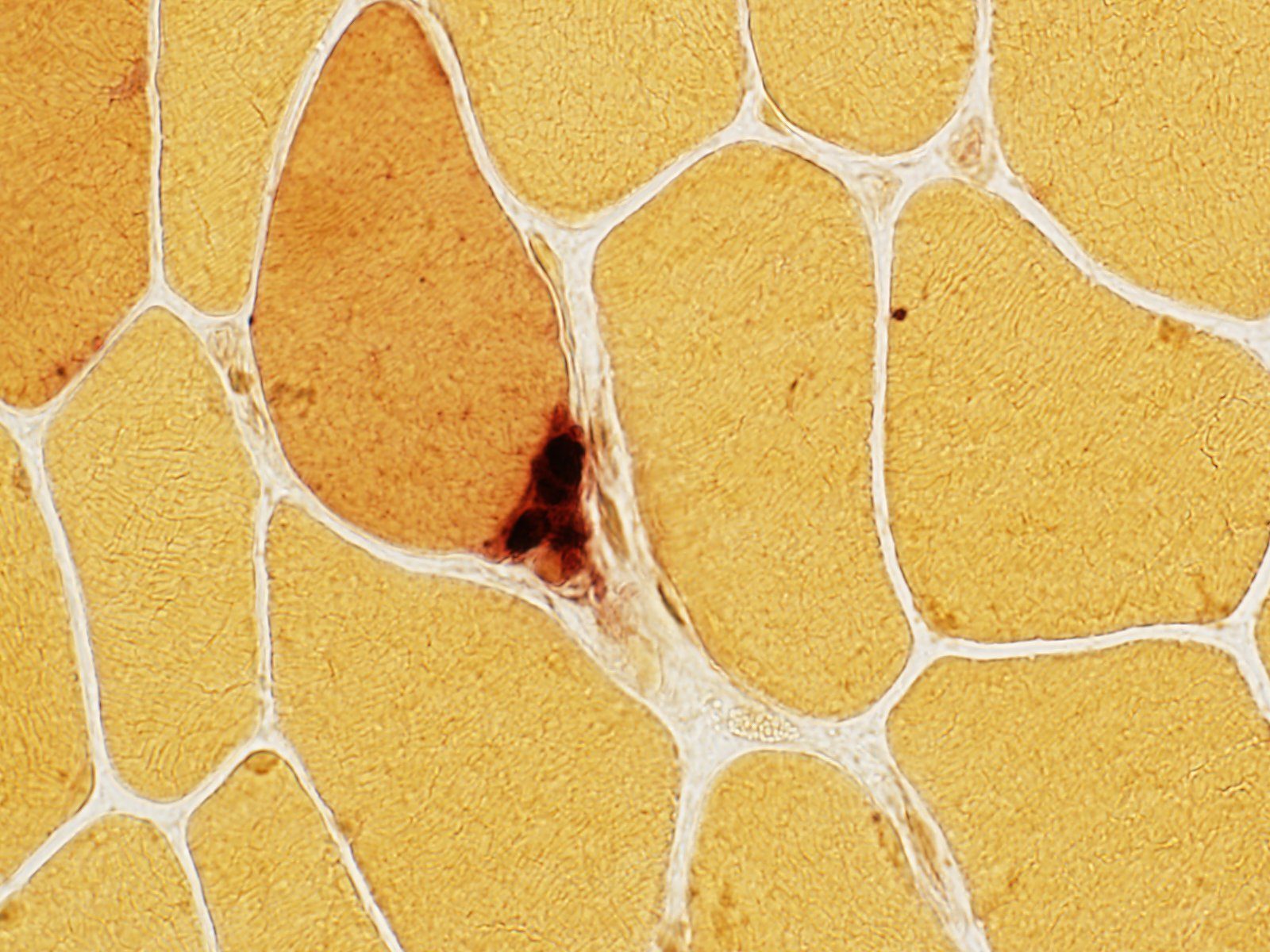
Armanni-Ebstein Lesion
Armanni-Ebstein lesion, originally described by Luciano Armanni in 1872, is characterized by vacuolization and PAS-positive glycogen accumulation within the cytoplasm…
Diagnose This!
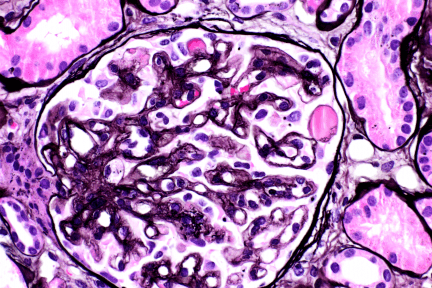
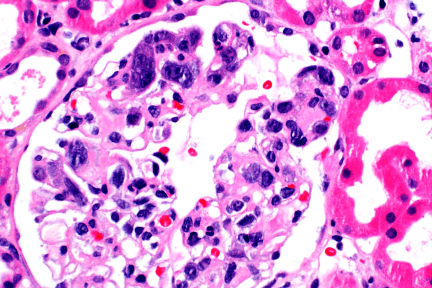
Diagnose This (October 10, 2022)
This is the biopsy of a 47-year-old female with cervical cancer, on anti-VEGF therapy, with proteinuria and normal renal function.…
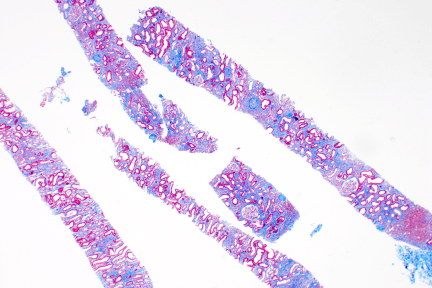
Diagnose This (September 26, 2022)
This is the biopsy from a 73-year-old with AKI and normal bone marrow biopsy done for investigation of anemia and…
Diagnose This (September 19, 2022)
In a 26-year-old obese Black female with no significant PMH and elevated creatinine, what is your top diagnosis? …
Podcast Episodes
Popular Subjects
Search & Filter All Posts