An elderly patient presents to nephrology for a rising creatinine. Baseline creatinine was 2.1 mg/dl six weeks prior but is now 3.4 mg/dl. He has poorly controlled diabetes and moderately well-controlled hypertension. Work up revealed a MGUS with positive IgG Lambda. Biopsy performed for kidney injury and to determine if there is a renal component related to his MGUS (r/o MGRS).
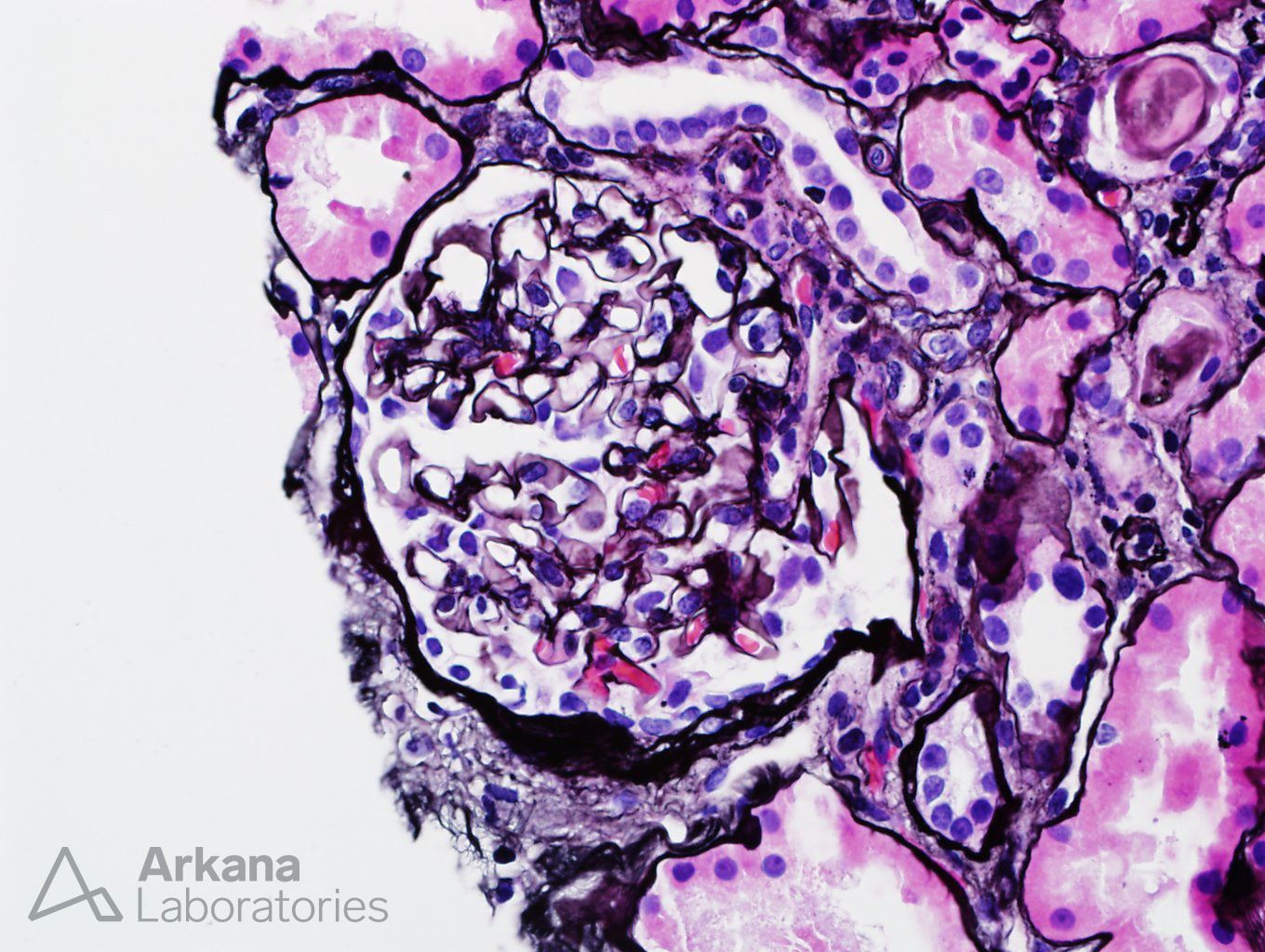
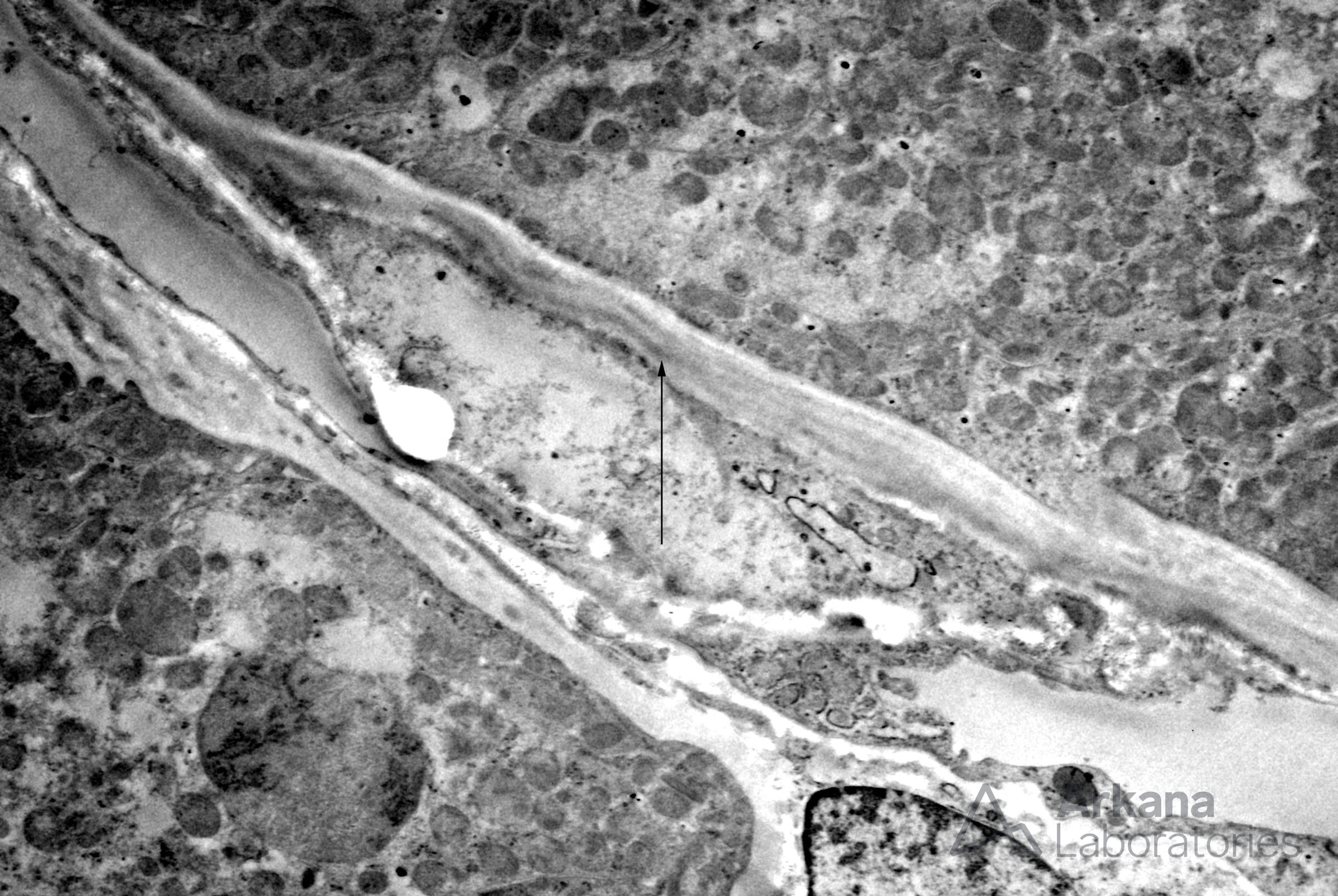
Electron microscopy revealed only irregular electron densities along the tubular basement membranes. No powdery deposits were found.
Diagnosis:
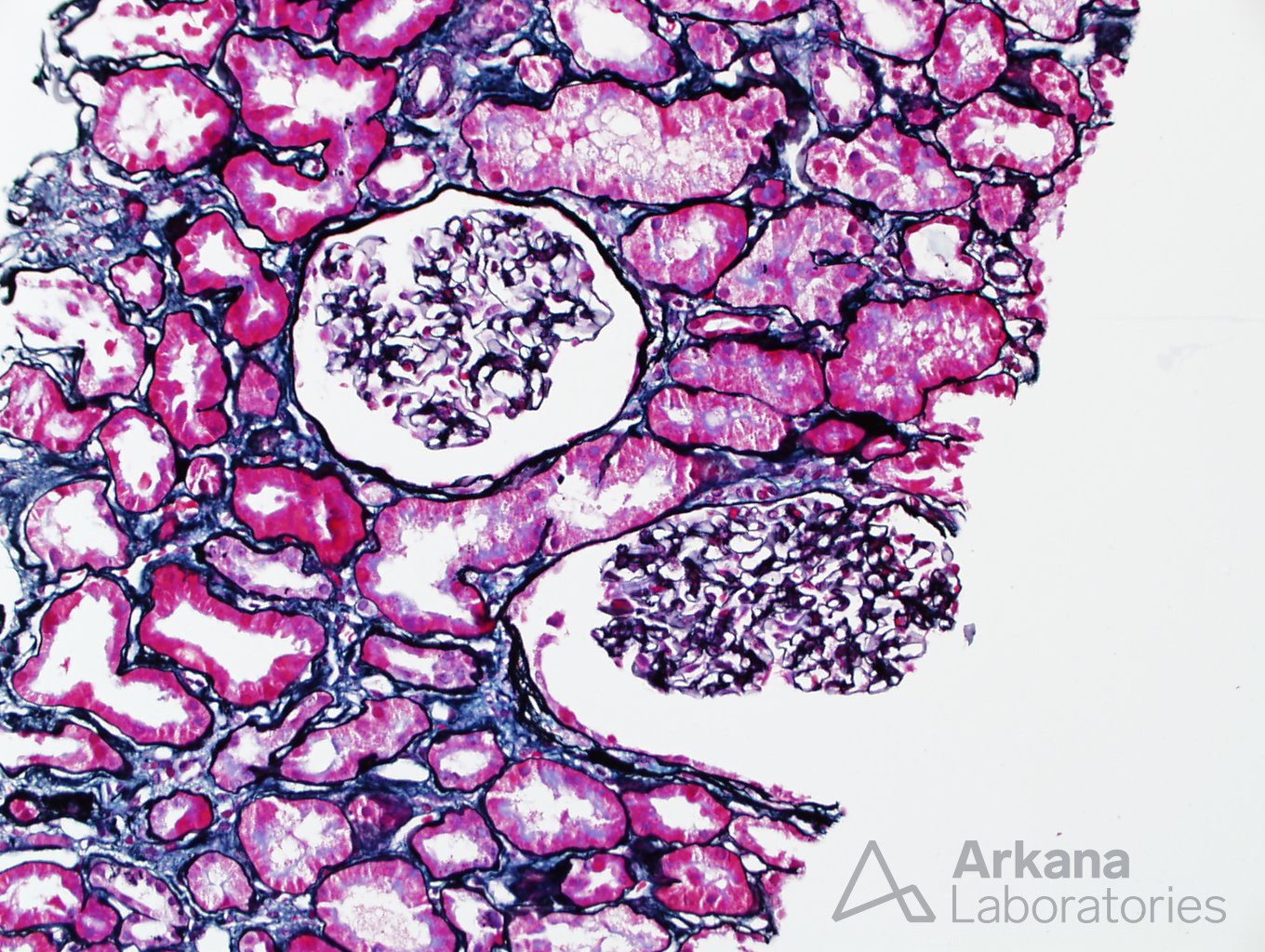
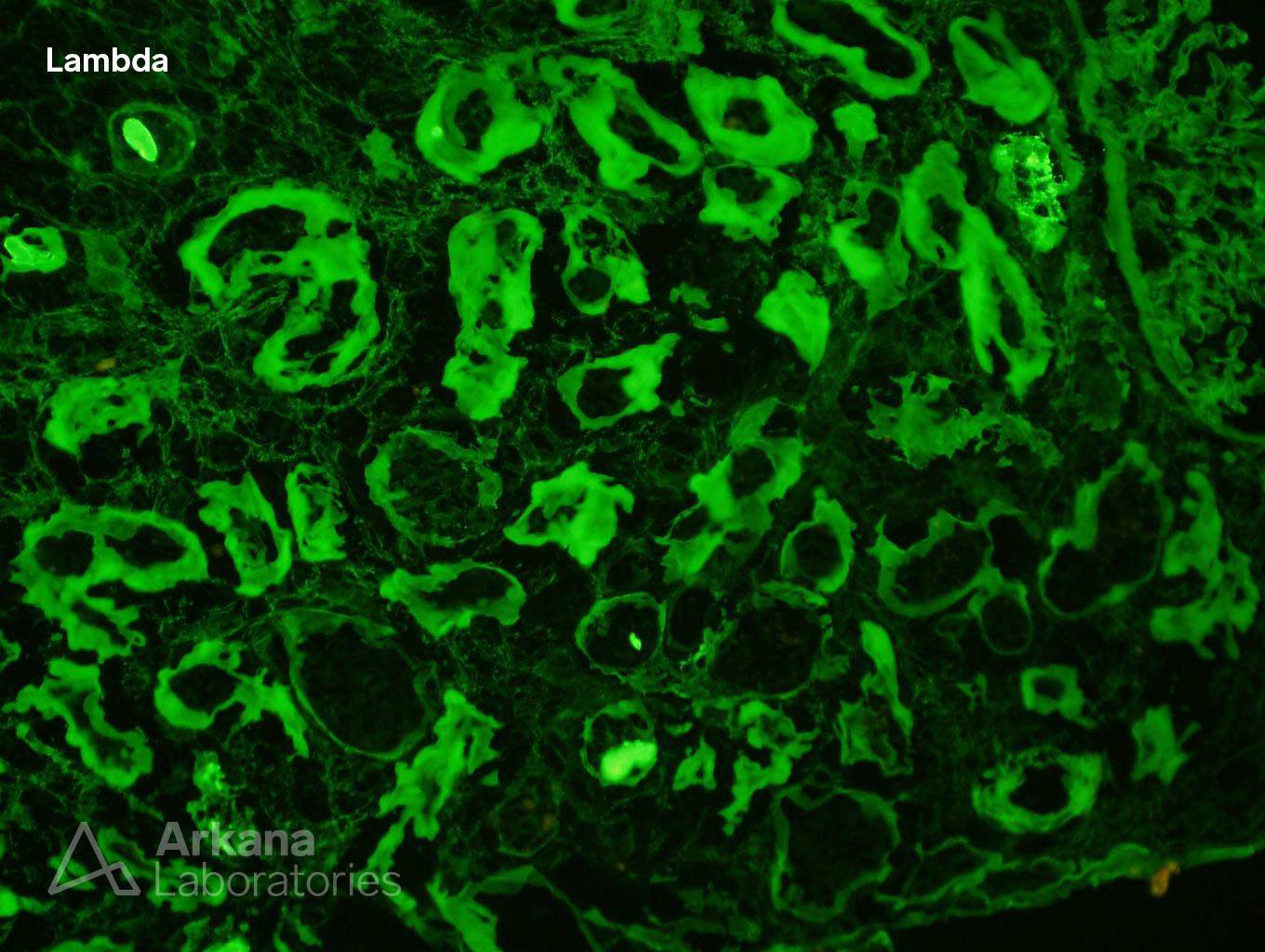
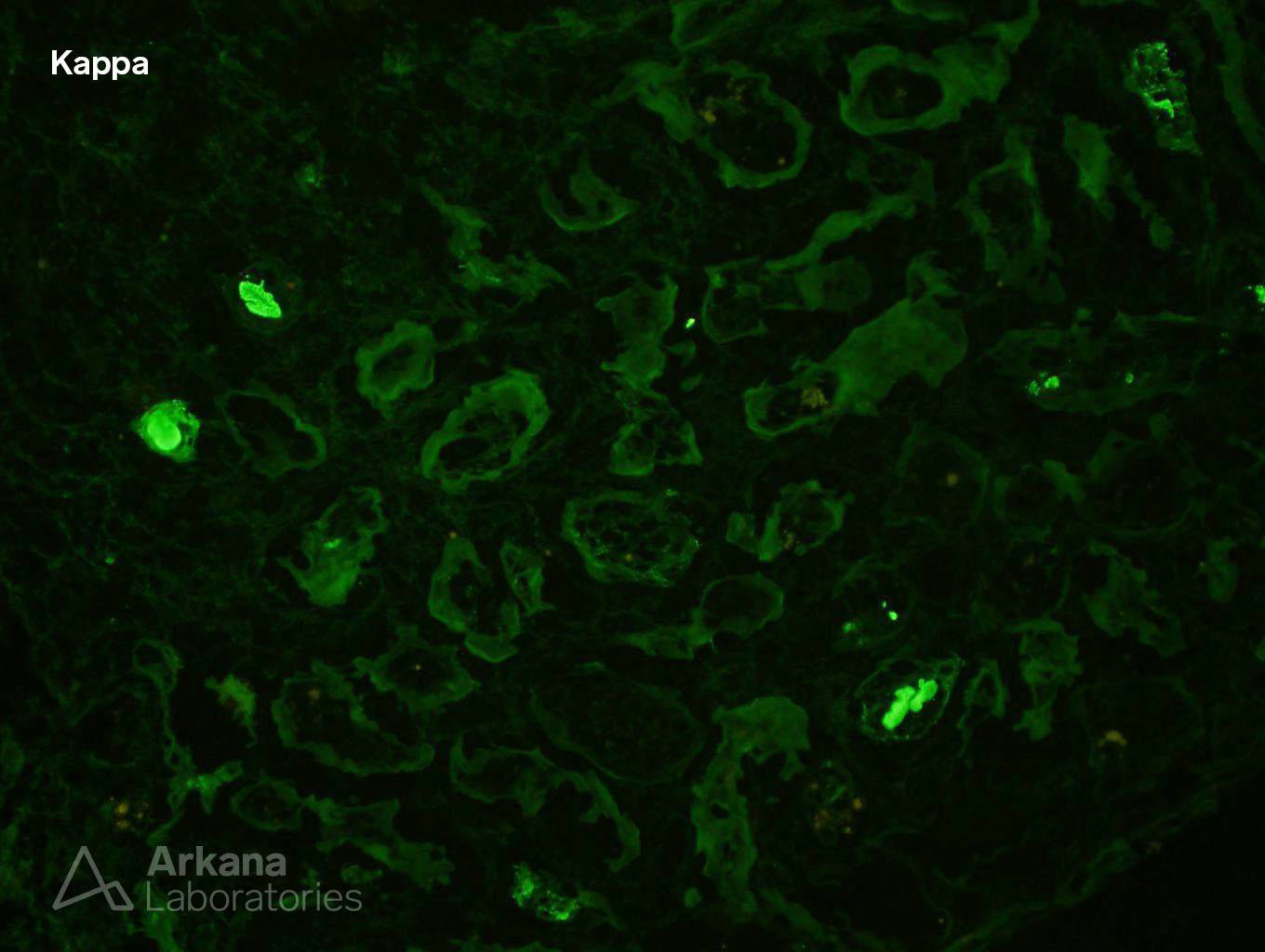
Immunofluorescence Features Suggestive of Light Chain Deposition Disease, Lambda Light Chain Type
Interstitial Fibrosis, Mild
Arteriosclerosis, Severe
Follow Up:
Bone marrow biopsy contained >20% plasma cells. Despite the lack of electron microscopic features present in fully developed cases of LCDD, the renal biopsy changes are sufficient to characterize this as a monoclonal gammopathy of renal significance (MGRS). Why? The IF pattern is typical of LCDD and there is evidence of renal injury clinically. Detailed examination for other causes of acute kidney injury yielded nothing. The patient was referred back to the Oncologist who will determine the next diagnostic and therapeutic steps.
Discussion:
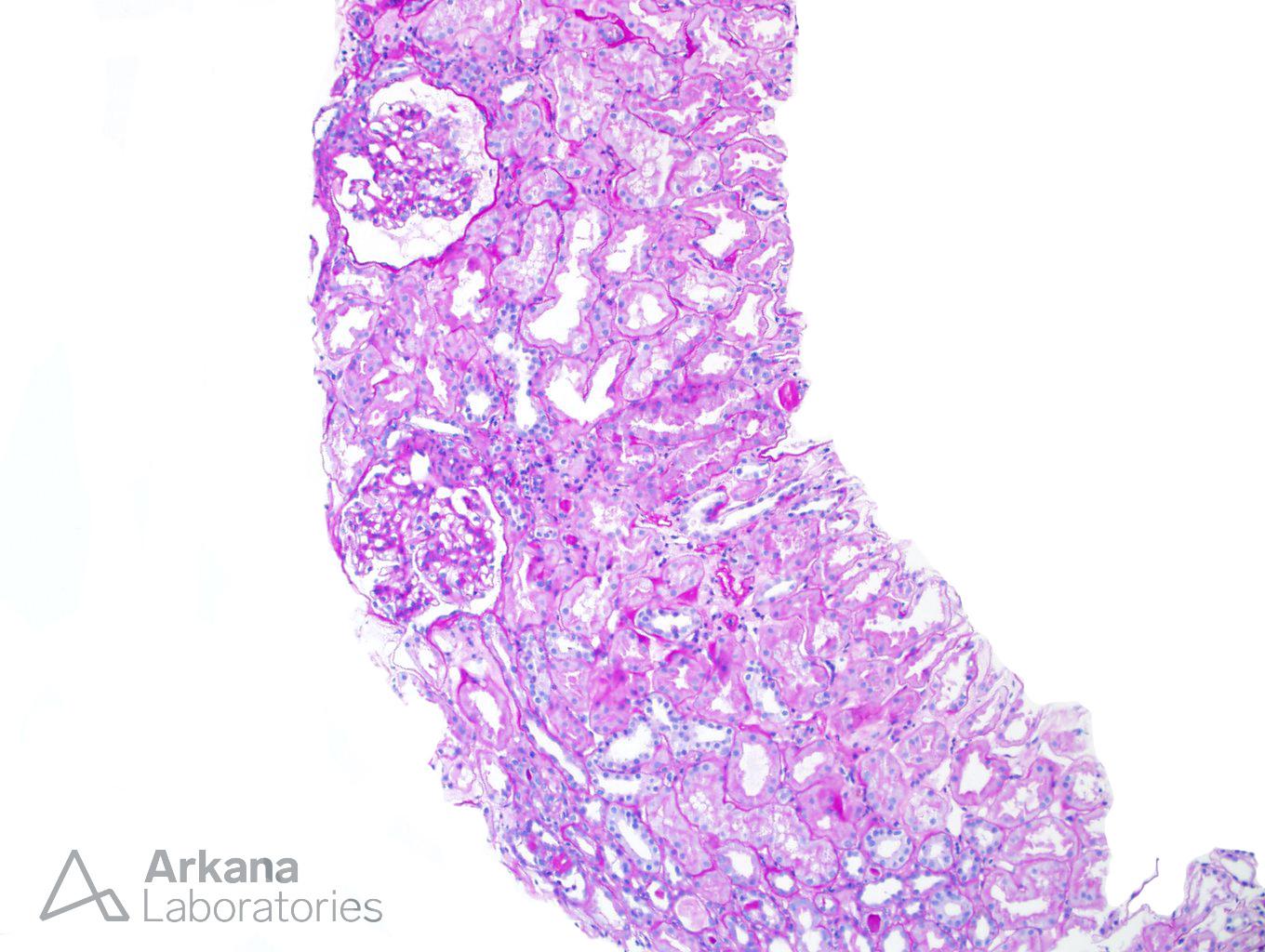
Light Chain Deposition Disease (LCDD), also called Monoclonal Immunoglobulin Deposition Disease (MIDD), is characterized by thickened tubular basement membranes (TBMs) and nodular glomerulosclerosis by light microscopy (LM). Immunofluorescence microscopy (IF) shows the monoclonal nature of the disease with linear deposits of either kappa or lambda light chains along the TBMs, the glomerular basement membranes and within the mesangium. Electron microscopy (EM) demonstrates the light chain deposition as powdery deposits along TBMs, GBMs and in the expanded mesangial areas. These diagnostic criteria are seen in cases that are well along in there course with the classic pattern of LCDD. But in this case, though the IF features strongly suggest LCDD, the corroborating EM features are absent. The renal biopsy shows none of the classic LM features of LCDD. In fact, the only changes on LM are arteriosclerosis and mild interstitial fibrosis. By EM, there are essentially no changes. Particularly no TBM deposits are seen despite an extensive search. Still, the characteristic IF pattern strongly suggests LCDD. In the setting of a diagnosis of multiple myeloma and a rising creatine, and after a thorough examination for other causes of acute renal injury was negative, the light chain deposition is thought to be the most likely cause of the renal injury.
References:
1. Gokden N, Barlogie B, Liapis H: Morphologic heterogeneity of renal light-chain deposition disease. Ultrastruct Pathol 2008, 32:17-24. https://www.ncbi.nlm.nih.gov/pubmed/18300034
2. Larsen CP, Bell JM, Harris AA, Messias NC, Wang YH, Walker PD: The morphologic spectrum and clinical significance of light chain proximal tubulopathy with and without crystal formation. Mod Pathol 2011, 24:1462-9. https://www.nature.com/articles/modpathol2011104?foxtrotcallback=true
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.