Monday
Did you know Fibrillary Glomerulopathy was described in the 1980s? While case reports existed before, in 1983 a series describing an unnamed renal disease was published. In 1987, the name fibrillary GN was coined in a second small case series.
https://www.ncbi.nlm.nih.gov/pubmed/6359891
https://www.ncbi.nlm.nih.gov/pubmed/3106698
Tuesday
Fibrillary GN has an overall poor prognosis. However, more recent studies stratify this more with somewhat consistent percentages of responders, progressive disease, and progression to ESKD.
https://www.ncbi.nlm.nih.gov/pubmed/28161700
https://www.ncbi.nlm.nih.gov/pubmed/21441134
Rituximab has become a common tx in fibrillary glomerulopathy. Data comes from small, uncontrolled case series but it appears to produce renal response in a subset of patients. Larger, controlled studies are sorely needed to determine tx superority.
https://www.ncbi.nlm.nih.gov/pubmed/23759297
https://www.ncbi.nlm.nih.gov/pubmed/24867652
Wednesday
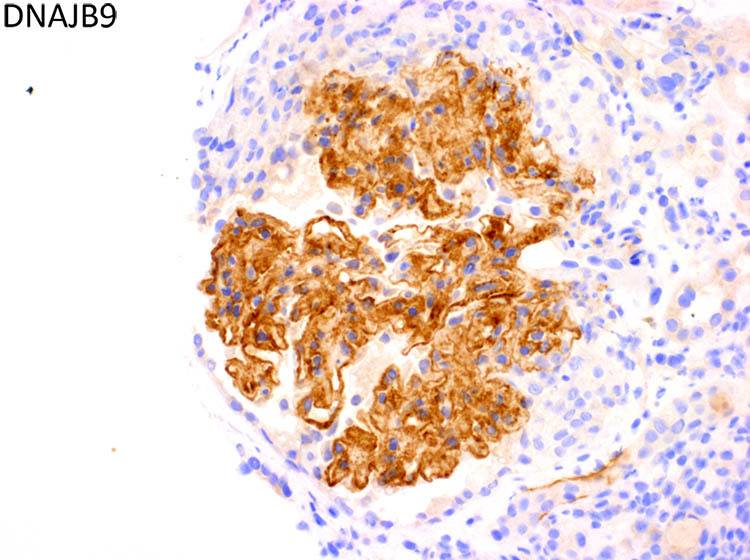
DNAJB9 is a recently discovered biomarker of fibrillary glomerulopathy. This discovery has already led to development of tissue biomarker stains. Could DNAJB9 represent a potential target for pharmacologic intervention?
https://www.ncbi.nlm.nih.gov/pubmed/29340314
https://www.ncbi.nlm.nih.gov/pubmed/29097624
https://www.ncbi.nlm.nih.gov/pubmed/29097623
Thursday
There are now emerging subtypes of fibrillary glomerulonephritis with subtle variations on biopsy such as Congophilic fibrillary glomerulonephritis and light chain restricted fibrillary glomerulonephritis.
https://pubmed.ncbi.nlm.nih.gov/33912743/
https://pubmed.ncbi.nlm.nih.gov/29866458/
A small percentage of fibrillary glomerulonephritis cases show monotypic light chain staining however, a recent study has suggested that the majority of these are not associated with monoclonal gammopathy.
https://pubmed.ncbi.nlm.nih.gov/32622524/
Recently, there has been an association with HLA-DR7 and fibrillary glomerulonephritis.
https://pubmed.ncbi.nlm.nih.gov/32775835/
https://pubmed.ncbi.nlm.nih.gov/33102980/
Friday
Fibrillary glomerulopathy is a disease undergoing rapid change. In just ten years several clinical disease state associations have been defined, a new treatment paradigm has emerged, new diagnostic tests on renal biopsy have been discovered, and the beginnings of the molecular pathogenesis of the disease have been found.
In the coming years, I hope continued research will help us answer a few important questions. First, no controlled, large scale, collaborative trials exist that prove treatment superiority in this disease and are sorely needed. Next, I hope that the discovery of DNAJB9 as a biomarker of this disease ignites a flurry of interest that leads to a more complete understanding of the molecular pathogenesis of this disease. When we have a fuller understanding of treatment superiority and an expanded knowledge of the pathogenic mechanisms behind fibrillary GN we will be in a place ripe for development of targeted therapies and will have the ability to compare them with current treatment options. And, while this still feels a ways off, if the last ten years are any predictor, it may come faster than we think.
Below you will find an abbreviated list of studies in fibrillary GN for your perusal. This list is not comprehensive or authoritative but it provides a good base for getting to know this disease. It takes less than 30 minutes to read through all the article abstracts and at the end, you will have a much more comprehensive understanding of fibrillary GN, current rationale for rituximab treatment, outcome and prognosis, side effects, and our current level of understanding of DNAJB9 and its intersection with fibrillary GN.
Early Literature
- While multiple cases report likely dealing with fibrillary GN exist before, this is the first case series I could find dealing with fibrillary GN. In this series, the disease is not named and from the images, there is likely significant overlap with immunotactoid glomerulopathy. https://www.ncbi.nlm.nih.gov/pubmed/6359891
- Four years after the previous study this case series coined the name ‘fibrillary glomerulonephritis’ and described the morphology of the disease. https://www.ncbi.nlm.nih.gov/pubmed/3106698
Outcomes and Case Series
- This is the most recent (as of early 2019) case series looking at 42 patients with outcomes and non-controlled treatment choices. https://www.ncbi.nlm.nih.gov/pubmed/28161700
- This is the largest case series detailing outcomes and non-controlled treatment choices in 66 patients. Of note, this paper has a strong pathology focus and refines fibrillary GN into the disease we diagnose today. https://www.ncbi.nlm.nih.gov/pubmed/21441134
- As we saw in the initial case series describing fibrillary GN there was, for many years, an uncomfortable overlap between fibrillary GN and immunotactoid GN. This case series includes 61 patients and is predominantly focused on differentiating the two diseases. As it was written in 2003, the previous paper is a better representation of the morphologic features of fibrillary GN as they are used today. https://www.ncbi.nlm.nih.gov/pubmed/12631361
- This is a case series of 16 patients that uses a three year follow up to establish outcomes. Unfortunately, the non-immunosuppressed group was too small to compare to the treatment group and this hinders the paper. Regardless, it is informative and details a somewhat worse prognosis than more recent papers. https://www.ncbi.nlm.nih.gov/pubmed/22553112
- This case series from 2013 describes 27 patients with average follow up of 46 months and describes several treatment groups. Although not controlled and sample sizes too small to statistically compare, it is informative. https://www.ncbi.nlm.nih.gov/pubmed/23759297
-
Large case series of 266 cases of fibrillary glomerulonephritis. https://pubmed.ncbi.nlm.nih.gov/31685544/
Treatment of Fibrillary Glomerulopathy with Rituximab
- This is the same study as #5 on the previous list. Of the 27 adults patients, seven were treated with rituximab of these five showed renal response at 46 months. https://www.ncbi.nlm.nih.gov/pubmed/23759297
- This is the largest case series of patients with fibrillary GN treated with rituximab that I found. It consists of 12 patients followed for an average of 38 months, four were non-progressors, three had progressive renal function decline, and five reached ESKD. https://www.ncbi.nlm.nih.gov/pubmed/24867652
- This is an older case series (2008) of three fibrillary GN patients treated with rituximab and followed for 27 months. All showed a marked reduction in proteinuria and preservation of renal function. https://www.ncbi.nlm.nih.gov/pubmed/18823685
- This small case report details two patients with fibrillary GN, treated with rituximab, and followed for 24 months. Both showed preserved renal function at 24 months and initial, significant reduction of proteinuria. One patient developed an abrupt rise in proteinuria at the end of the follow-up period and recurrence was suspected. https://www.ncbi.nlm.nih.gov/pubmed/24831880
Side Effects and Reported Concerns (this is just a very small selection)
- Case report describing clinical recurrence of fibrillary GN in the context of B-cell reconstitution after rituximab therapy. https://www.ncbi.nlm.nih.gov/pubmed/30423930
- Case report of pulmonary disease associated with rituximab therapy in a patient with fibrillary GN. While this is a well-known complication in rheumatologic diseases, it is less commonly reported in the context of fibrillary GN. https://www.ncbi.nlm.nih.gov/pubmed/26064515
- Case report of a patient with spontaneous regression fibrillary GN clinically and histologically. Only reported histologic resolution of fibrillary GN I’m aware of. https://www.ncbi.nlm.nih.gov/pubmed/29225801
- Case series of 18 cases of Congophilic fibrillary GN. Prior to the discovery of DNAJB9 this entity was very difficult to stratify for pathologists and still causes significant confusion despite better evaluation methods now available. Misclassification into amyloidosis is very easy in this entity. https://www.ncbi.nlm.nih.gov/pubmed/29866458
- Fibrillary GN can represent an MGRS, but the majority are not MGRS. https://www.ncbi.nlm.nih.gov/pubmed/26735145
-
With the advent of DNAJB9 and MGRS, new diagnostic algorithims are being proposed for diagnostics of unusual variants of fibrillary glomerulonephritis and new data is emerging regarding a small subset of patients with fibrillary glomerulonephritis representing MGRS.
-
An association between HLA-DR7 and fibrillary glomerulonephritis has been identified.
DNAJB9
- Exceptional paper from the Mayo Clinic group detailing their discovery of DNAJB9 as a specific and sensitive biomarker via immunohistochemistry for fibrillary GN. https://www.ncbi.nlm.nih.gov/pubmed/29340314
- DNAJB9 as a potential autoantigen in fibrillary GN and glomerular proteome analysis. https://www.ncbi.nlm.nih.gov/pubmed/29097624
- DNAJB9 as a novel biomarker, proteomic analysis of fibrillary GN and detailed molecular discussion. There is a mistake in this paper, however. It says “no unique histologic biomarkers for diagnosing FGN have been identified,” which is incorrect as the Mayo paper #1 above appeared around 5 months prior to this one. https://www.ncbi.nlm.nih.gov/pubmed/29097623
- This paper describes DNAJB9 and its inducible function by p53 via the Ras/Raf/ERK pathway. This paper is from 2015 and came shortly after the discovery of DNAJB9 but before any association between DNAJB9 and fibrillary GN. https://www.ncbi.nlm.nih.gov/pubmed/25146923
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.